Ending Unequal Treatment: Strategies to Achieve Equitable Health Care and Optimal Health for All (2024)
Chapter: 2 The Health Care System Within a Larger Societal System
2
The Health Care System Within a Larger Societal System
The U.S. health care system exists within the larger U.S. society and interfaces with this much larger societal system that shapes how health care is organized, financed, delivered, and accessed and also influences how and whether the health care system is held accountable to achieve optimal and equitable health care outcomes for all (see Figure 2-1).
Differences in health by race and place are well documented (Barber, 2020), and individuals embody such differences (Krieger, 2005) as they enter and navigate the health care delivery system (Kelley et al., 2005). Health care influences and affects many of these historical and current societal forces, and what happens in the larger societal system affects what happens in the health care system. Therefore, understanding the key external societal forces that interface with the health care system requires a multilevel, multifactorial, biopsychosocial approach that recognizes the intersecting and interacting determinants across the life course (Trickett and Beehler, 2013). This chapter discusses the key societal forces external to the health care system that interface with it to contribute to racial and ethnic health care inequities (shown in the committee’s conceptual framework in Chapter 1, Figure 1-3). Moreover, as emphasized by the Healthy People 2030 framework, merely addressing factors contributing to inequitable health care access and quality alone cannot improve the factors contributing to poor health and health care outcomes across and between social groups.
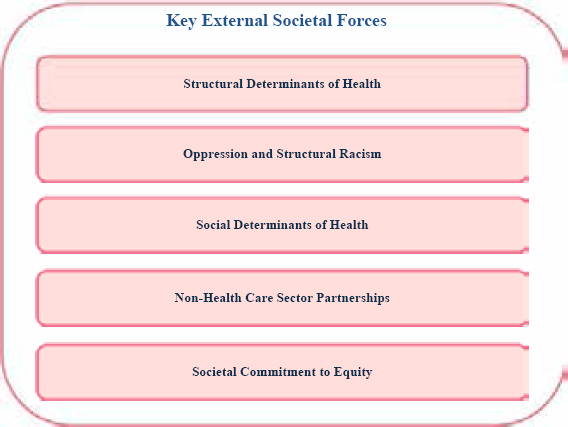
NOTE: The key external societal forces act individually, intersect with one another, and constantly interact with the domains in the health care system.
Ameliorating the factors preventing individuals and social groups from achieving their best health possible or attaining their full health potential requires also addressing the societal, environmental, economic, and political forces that develop and exist well before individuals enter the health care system. Research has shown how these social, political, economic, and environmental conditions that adversely impact racially and ethnically minoritized groups consistently lead to health and health care inequities (Lucyk and McLaren, 2017; Plamondon et al., 2020; Taylor et al., 2016). As noted in Chapter 1, the committee acknowledges that terms used in this area of research have evolved over time and will continue to do so as further insights are gained and society and demographics shifts. As explained in Chapter 1, this report uses “inequities” instead of “disparities” except when citing a publication that explicitly measured disparities. The committee is also aware that health—a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity—and health care—the services provided to individuals, families, and communities for the purpose of promoting, maintaining, or restoring health across settings of care—are different but inextricably linked. Furthermore, this report uses “health care system” (activities related to the delivery of care across the continuum of care) to
describe the U.S. health care system as a whole and individual health care systems and “health” when discussing outcomes.
This chapter considers a variety of societal factors that impact health, including the social norms, laws, and policies that set the stage for upstream systems of oppression, including structural racism, structural sexism, heterosexism, classism, cissexism, xenophobia, colonialism, and ageism. Also, this chapter covers a variety of societal factors that impact health, including the social norms, laws, and policies that set the stage for upstream systems of oppression, such as structural racism, structural sexism, heterosexism, classism, cissexism, xenophobia, colonialism, ageism, and ableism (Brown and Homan, 2022). While this report is focused on race and ethnicity, these other forms of oppression intersect in various ways to shape an individual’s health outcomes, which is defined as structural intersectionality (Brown and Homan, 2022). These upstream structural determinants of health, which are shaped by norms, laws, and policies, set the context to develop social determinants of health (SDOH) (conditions in the environments in which people live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks) that operate at the population level. SDOH create the context for a patient’s health-related social needs (HRSNs) (social and economic needs that affect individuals’ ability to maintain their health and well-being), which operate at the individual level. In addition, health care systems interact with communities and non–health care entities to powerfully shape health and health care outcomes. Finally, a societal commitment to equity is an external force that is essential to eliminating health inequities and needs to be cultivated and nurtured.
STRUCTURAL DETERMINANTS OF HEALTH
Structural determinants of health are defined as “cultural norms, policies, institutions, and practices that define the distribution (or maldistribution) of the SDOH (Crear-Perry et al., 2021).” Policies are the laws, codes, and rules governing our society—and social and cultural norms are the values, attitudes, and beliefs about who in society is worthy of advantage and who is worthy of disadvantage. Social and cultural norms can represent racist, classist, ableist, misogynistic, xenophobic, and other hateful ideologies, but they are most commonly powered by implicit biases of which people are not consciously aware (Shim and Compton, 2020). Social norms and public policies interact with each other to create an unfair and unjust distribution of opportunity in society (Shim and Compton, 2020). For example, negative social norms in the 1980s led to “moral panic” about crack cocaine, a drug commonly associated with Black people (Isom et al., 2021). Black people who used crack cocaine experienced highly gendered
discriminatory social norms (perpetuated by the media) in which Black men were seen as violent criminals and Black women were depicted as depraved mothers who prioritized the drug over their children’s welfare.
The Anti-Drug Abuse Act of 1986 created a 100-to-1 disparity between crack and powder cocaine: 1 gram of crack cocaine carried the same federal prison sentence as 100 grams of powder cocaine, despite these drugs being the same chemical compound.1 This unfair and unjust policy, based on biased social norms, activated exposures to many adverse SDOHs, including mass incarceration (Bailey et al., 2021). Incarceration limited people’s opportunities for employment upon release, triggering area-level and individual poverty, food insecurity, housing insecurity, problems accessing health care tied to employment, and neighborhood disorder and exposure to violence. Furthermore, the interaction of these social norms and public policies created intergenerational effects (e.g., having a parent who is incarcerated is an adverse childhood experience [ACE]). This example highlights how unfair and unjust policies lead to differential health impacts from SDOHs. Social norms inform public policies around drug use, including criminalization of certain drugs (e.g., crack cocaine) and access to evidence-based medical treatments for others (e.g., prescription opioids) (Netherland and Hansen, 2017). Although rates of opioid use disorders are relatively consistent across racial groups, early access to medication-assisted therapies for prescription opioid use disorder was disproportionately more available to White people than Black and Latino/a people (Netherland and Hansen, 2017).
Social norms and values drive laws and policies and how they are implemented. For example, the United States values a market-driven economy, which is a dominant paradigm for society. Market forces in the health care system incentivize efforts to attract only the best payers and healthy patients. Equity is not prioritized compared to optimizing service revenue based on organizations’ strategies, cultures, funding, processes, people, leadership, and systems (Powers et al., 2021). This fundamental misalignment of goals yields a vicious cycle that undervalues primary prevention and overvalues biomedical treatment of disease based on payment. Market-driven systems lead to significant differences in outcomes according to the ability to pay (as an example of how social norms have influenced the health care sector, see Box 2-1 for a discussion on health care financing and insurance design).
___________________
1 See https://www.ussc.gov/sites/default/files/pdf/training/annual-national-training-seminar/2009/016b_Road_to_1_to_1.pdf (accessed April 29, 2024).
BOX 2-1
Health Care Financing and Insurance Design
Market-driven forces influence health care and other U.S. institutions, such as higher education or housing. Market-driven differences in payments for services and market-driven socioeconomic determinants of health influence and perpetuate racial and ethnic inequities. Health care providers are paid less for care delivered to patients whose insurance is Medicare or Medicaid, relative to those privately insured by employers. This differs from other national health care systems, where payment is standardized due to a larger role for universal coverage systems (Pulok et al., 2020). Hospitals paid according to nationally or regionally negotiated rates are more likely to be government-owned, and physicians are more likely to be salaried rather than paid according to volume or type of insurer. The U.S. system of unequal reimbursement by itself is not expected to lead to racial inequities in health care provision. Instead, the systematically higher representation of minoritized populations in lower-reimbursement health care, particularly in Medicaid, is a historical incentive to provide unequal treatment. Even though out-of-pocket costs are lower in Medicaid than in private insurance, the amount that providers receive is much lower, often for providing care in more challenging circumstances and to less-resourced patients.
The financial forces of insurance system differences in reimbursements for care intersect with other historical structures and health care cultures that produce inequities by race and ethnicity. Examples of downstream pathways through which these macro-level factors contribute to such inequities in health include early life trauma, lifelong chronic stress, and result in direct impact on health or indirect impact through health behaviors.
Another area of market-driven inequities is out-of-pocket costs, even in a universal insurance system where providers are paid the same. Cancer (and other chronic illnesses) are illustrative examples. Financial toxicity from treatment for advanced cancer has disparate impacts among minoritized populations (Rotter et al., 2019), affecting quality of life (Arastu et al., 2020). Among Medicare beneficiaries with advanced cancer, inequities in hospice appear to have closed, although variations exist by age, cancer, and place (Estrada et al., 2021; Mullins et al., 2021; Samuel-Ryals et al., 2021).
OPPRESSION AND STRUCTURAL RACISM
Oppression and Health Outcomes
Oppression is defined as a state in which people have unequal power and the process by which dominant groups use power to subjugate dominated groups (David et al., 2019). While racism is one form of oppression based on membership in racial and ethnic groups (David et al., 2019), many other forms of oppression intersect and work synergistically to keep dominant groups in power and keep subjugated groups powerless. One investigator has identified “five faces of oppression”: exploitation, marginalization, powerlessness, cultural imperialism, and violence (Young, 2014).
Over the last 2 decades, empirical studies have documented the relationship between oppression and health (Jemal, 2018). Toxic stress and trauma from oppression adversely affect psychological and physical health and well-being. Furthermore, health care providers’ oppressive beliefs and behaviors can lead to lower-quality care and poor outcomes (Barr, 2014). Additionally, ample evidence suggests that chronic exposure to various forms of oppression leads to accelerated aging and the earlier onset of poor health outcomes, a phenomenon known as “weathering” (Geronimus, 1996), which is more pronounced in racially and ethnically minoritized groups, groups with lower socioeconomic status, and those living in segregated neighborhoods (Forde et al., 2019).
Structural Racism2 and Health Outcomes
Although multiple societal factors affect health and health care inequities, it is the health and health care differences by race and ethnicity that remain the most persistent and difficult to address (NASEM, 2017; Williams and Mohammed, 2009). Specifically, race and racism have played and continue to play such a significant role in structuring our society that efforts to affect the drivers of health and health care inequities without addressing historical and contemporary racism are unlikely to be effective (Bailey et al., 2017; NASEM, 2017). Research has established multiple pathways by which racism harms health, including adverse physical, social, and economic exposures, maladaptive coping behaviors, and stereotype threat (Abdou et al., 2016; Blair et al., 2013; Fullilove, 2016; Paradies et al., 2015; Slopen et al., 2016). These exposures accumulate over the life course and across generations (Bailey et al., 2017). However, some investigators contend that most studies investigating the association between racism and
___________________
2 The National Academy of Medicine is developing a series of special publications on how systemic and structural racism perpetuate oppression. See https://nam.edu/programs/culture-of-health/systems-impact-special-publication/ (accessed on April 29, 2024).
health have focused on interpersonal racial and ethnic discrimination, with few studies attempting to explain the health effects of structural or systemic racism on population health (Bailey et al., 2017).
For this report, the committee specifically emphasizes structural racism, understanding that “systemic racism” is often used interchangeably with it and that some scholars note subtle differences in terminology (Braveman et al., 2022). By focusing on structural racism over all other types of racism, the committee considers the foundational elements that drive racism in systems, both within and outside of health care delivery, and how these interact with systems that impact the health care system. Although this chapter discusses structural, interpersonal, and internalized racism, many other types of racism create pathways to health care inequities, including institutional (see Chapter 5) and scientific (see Chapter 7) racism.
Structural racism is defined as “the normalization and legitimization of an array of dynamics—historical, cultural, institutional, and interpersonal—that routinely advantage whites while producing cumulative and chronic adverse outcomes for people of color” (Lawrence and Keleher, 2004). Many studies characterize its role in driving inequitable health and health care outcomes among minoritized populations (Bailey et al., 2017; Hailu et al., 2022; Muramatsu and Chin, 2022; O’Brien et al., 2020; Wang et al., 2023; Wien et al., 2023; Yearby et al., 2022). For example, residential segregation, a direct result of the structurally racist policy of redlining3 that designated Black and immigrant neighborhoods as less worthy of services, leading to widespread reductions in home value, home ownership rates, access to credit, and community investment over time (Aaronson et al., 2021). Although Congress passed legislation prohibiting redlining in 1968,4 the legacy of redlining and residential segregation are still associated with inequitable health and health care outcomes today. One study, for example, examined eight cities in California and documented a statistically significant increase in emergency department visits for asthma-related care in historically redlined, predominantly Hispanic and Black communities (Nardone et al., 2020).
Significant challenges arise in operationalizing and measuring structural racism, as established measures often examine single dimensions (e.g., the index of concentration at the extremes (Krieger et al., 2018) or single domains (e.g., residential segregation) (Chantarat et al., 2021).
___________________
3 Redlining is a policy developed by the federal government’s Homeowners Loan Corporation during the 1930s that denied people loans because of where they live, regardless of whether they were qualified. It was meant to deprive Black people, and later Latino/a people and immigrants, of homeownership.
4 See https://www.govinfo.gov/content/pkg/COMPS-343/pdf/COMPS-343.pdf (accessed March 29, 2024).
However, in recent years, significant progress has been made in measuring structural racism, including published guidelines for how to measure structural racism more effectively (Adkins-Jackson et al., 2022; Brown and Homan, 2022; Furtado et al., 2023; Hardeman et al., 2022). A comprehensive review of empirical research connecting structural racism to poor health outcomes exists. The section that follows highlights some of such studies.
Interpersonal Racism and Health Outcomes
Interpersonal racism is defined as racist interactions between individuals (Paradies, 2006). Although this report emphasizes the role of structural racism as a contributor to inequitable health and health care outcomes, this is rarely the form of racism that first comes to mind for most people. Structural racism is most commonly implicated in creating health and health care disparities, but interpersonal racism also plays a role, with research highlighting this connection between perceived interpersonal racism and the risk of stroke in Black women (Sheehy et al., 2023). A comprehensive systematic review and meta-analysis found that interpersonal racism was associated with many adverse health outcomes, including poorer mental health (including depression, anxiety, and psychological stress), physical health (including hypertension and obesity), and general health (Paradies et al., 2015).
Discrimination, a behavioral outcome of interpersonal racism, includes discrimination mandated by law (de jure), such as Jim Crow laws that legalized racial segregation, and discrimination without legal basis but sanctioned by custom (de facto), such as the underrepresentation of women and minoritized populations in leadership roles in medicine (Shim and Compton, 2020). Data on discrimination and its impact on poor health outcomes are very robust (Williams et al., 2019). Additionally, xenophobia, a form of oppression and a specific form of discrimination, is defined as “attitudes, prejudices, and behavior that reject, exclude, and often vilify persons, based on the perception that they are outsiders or foreigners to the community, society, or national identity.”5 Studies have shown that xenophobia is responsible for poor mental health outcomes, including depression and physical violence, with compounding effects when intersectional oppressed identities are involved (Suleman et al., 2018). Xenophobic policies also contribute to poor health outcomes; research has shown, for example, that the Latino/a population in states with more exclusionary immigration
___________________
5 See https://publications.iom.int/system/files/pdf/international_migration_racism.pdf (accessed April 29, 2024).
policies (e.g., restricting opportunities and resources for immigrants) had higher rates of poor mental health days than Latino/a people in states with less exclusionary policies (Hatzenbuehler et al., 2017).
Implicit Bias and Health Outcomes
Much of the relevant data on interpersonal racism’s impact on health care outcomes has focused on health care providers (HCPs). The role of their relationship with patients has been discussed in the context of increasing knowledge of implicit bias, the neurobiologically based, automatic attitudes and beliefs about particular social groups and their members (Hagiwara et al., 2020). These implicit biases can affect cognition (i.e., stereotypes), affect (i.e., prejudice), and behavior (i.e., discrimination) (Hagiwara et al., 2020).
The literature on implicit bias in health care settings is robust and has increased significantly in the 20 years since Unequal Treatment. A systematic review in 2017 found that physicians and nurses hold implicit biases at the same level as the general population (FitzGerald and Hurst, 2017). However, their implicit biases lead to poor health and health care outcomes for minoritized patients. Studies have shown that physicians’ high levels of implicit bias toward Black patients positively correlated with those patients’ negatively rating their interactions (Cooper et al., 2012) and identified implicit biases against Latino/a patients seeking health care, even when expressions of explicit bias are low (Blair et al., 2013). Effective longitudinal interventions exist for reducing implicit bias toward people of color, and experts have called for more widespread implementation in health care settings (Devine et al., 2012).
Internalized Racism and Health Outcomes
Despite significant evidence to support interpersonal racism’s impact on poor health outcomes and a growing body of evidence that structural racism adversely impacts health outcomes, less scientific attention has been paid to internalized racism (David et al., 2019), which is defined as “the individual inculcation of the racist stereotypes, values, images, and ideologies perpetuated by the White dominant society about one’s racial group, leading to feelings of self-doubt, disgust, and disrespect for one’s race and/or oneself” (Pyke, 2010). Evidence suggests an association with poor health outcomes, as studies have found that higher rates of internalized racism are linked to conditions such as depression (Mouzon and McLean, 2017), anxiety (Graham et al., 2016), cardiovascular disease (Chae et al., 2010), and premature death (Chae et al., 2014). A meta-analysis of the relationship between internalized racism and health reported a direct relationship with negative mental and physical health outcomes (Gale et al., 2020).
SOCIAL DETERMINANTS OF HEALTH (SDOH)
The SDOH, which occur downstream from structural determinants of health and structural racism, are the conditions in the environments in which people live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks (HHS Office of Disease Prevention and Health Promotion, 2024). Across the lifespan, these environments influence their health and how they navigate the health care system. The unequal distribution of health-promoting and -damaging resources in those environments, along with a myriad of historical and current societal forces, contributes to unequal health and health care outcomes across racial and ethnic populations (NASEM, 2017).
These inequities are the product of structural determinants of health (including oppression and structural racism), corresponding adverse SDOH, and the wider set of forces and systems shaping the conditions of daily life (Bundy et al., 2023; Ortega and Roby, 2021; Yearby et al., 2022). A cycle of inequities occurs with compounding effects: health inequities contribute to inequities in access to treatment resulting from the failure of the health care system to accommodate people from different cultures and people with health impairments (Dickman et al., 2017; Matin et al., 2021). For example, a person who has experienced a stroke might struggle to make an appointment by phone due to a speech impairment or be unable to climb the steps of a bus to get to an appointment as a result of partial paralysis. It has been reported that health and health care–related research and practice have no agreed-upon standards of what factors constitute the SDOH, so developing, implementing, and evaluating interventions to address SDOH remain challenging (Alderwick and Gottlieb, 2019). This report discusses SDOH using the domains conceptualized by Healthy People 20306: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context.
Economic Stability
Economic instability and lack of wealth directly contribute to poor health outcomes in a variety of ways. Wealth is related to access to income, assets, other resources, agency, and education (Park and Yang, 2021). A longitudinal analysis showed that increases or decreases in wealth after controlling for other factors explain within-person differences in mental and physical health (Park and Yang, 2021). In 2019, the median net worth of White families was roughly eight times that of Black families, despite only a 2:1 difference in income (Kent et al., 2022). Gaps in the wealth
___________________
6 See https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed April 29, 2024).
held by Black and Hispanic families compared to White families have remained unchanged for over 30 years (Kent et al., 2022). Researchers trace these long-standing differences to slavery, when enslaved Black people were viewed as property and assets of slaveowners. Upon the end of slavery, Black people were not given any additional assets or resources, and they continue to be affected by historical and modern-day discriminatory policies, including those related to land ownership and access to housing, education, retirement benefits, and credit (Kent et al., 2022). Investigators have also documented variation in intergenerational economic mobility, with significant advancement among Hispanic but not Black people (Chetty et al., 2020). None of the differences in family characteristics, including parental income, marital status, education, and wealth, or a person’s individual ability or motivation, explain much of the income gap between Black and White people (Chetty et al., 2020).
Significant differences exist in terms of access to employment and thus the ability to earn an income. For example, after recent rebounds in employment following the COVID-19 pandemic, the overall unemployment rate in 2022 was 3.6 percent (BLS, 2023). However, a closer look reveals important racial and ethnic inequities, with higher unemployment rates for American Indian and Alaska Native (AIAN) people (6.2 percent), Black people (6.1 percent), people of two or more races (5.5 percent), Latino/a people (4.3 percent) and Native Hawaiian and Other Pacific Islander (NHPI) people (4.0 percent) (BLS, 2023).
Multifactorial discriminatory factors help to explain these inequities in unemployment rates (BLS, 2023; Cutler, 2006). For those who are employed, research has shown that job rank, occupational conditions, and socioeconomic factors are positively associated with health outcomes (Hoven and Siegrist, 2013). Racially and ethnically minoritized populations were more likely to be deemed “essential workers” during the pandemic, requiring risk of exposure in the course of their daily work duties (Rogers et al., 2020). Furthermore, they are more likely to experience precarious employment, in which work is insecure, low pay, and without rights and protections (Frank et al., 2023). Unemployment has been associated with several poor mental health outcomes, including suicide (Amiri, 2022a), depression (Amiri, 2022b), and alcohol use disorder (Compton et al., 2014). The realities of managing economic instability include the stress imposed by the consistent struggle of navigating the constraints of attempting to pay for basic necessities without sufficient financial resources (Alhomsi et al., 2023).
Education Access and Quality
Early childhood education, parental educational attainment, and disciplinary actions influence students’ success in school. These factors affect racial and ethnic groups unevenly and lead to inequities in educational outcomes.
Research has shown that education is a powerful predictor of multiple health outcomes throughout the lifespan, including general health status, mortality, and depression (Cutler et al., 2006; Walsemann et al., 2013). Unfortunately, the U.S. educational system as it is designed reproduces inequities and hierarchies between racial and ethnically dominant and minoritized groups (Dumas, 2014; Duncan-Andrade and Morrell, 2008). Education policy has frequently framed these inequities as a racial achievement gap, without acknowledging the structural issues for minoritized children, including underresourced and underfunded schools (Kozol, 2012), harassment and harsh discipline (Wun, 2018), and attacks on self-worth (Dumas, 2014).
Health Care Access and Quality
While the health care system is discussed in greater detail throughout this report, access to quality health care is included in SDOH by many experts because it is shaped by economic and societal forces. Inequities in health insurance coverage are one of the main drivers of inequitable access. In 2022, uninsurance rates for non-elderly adults77 were highest for AIAN and Hispanic adults, at rates of 19.1 and 18.0 percent, respectively. The uninsurance rates were 12.7 percent for NHPI, 10.0 percent for Black, 6.0 percent for Asian, and 6.6 percent for White adults. (Hill et al., 2024). Additionally, rates of uninsurance were higher (and more inequitable) in states that did not expand Medicaid compared to states that did so (Hill et al., 2024).
Access to care for mental health and substance use disorders (SUDs) is also a concern, as Black (39 percent), Hispanic (36 percent), and Asian (25 percent) adults were less likely to use mental health services in 2021 than White adults (52 percent) (Hill et al., 2023). In 2023, only 35 percent of Black and Hispanic adults reported receiving SUD treatment, compared to 51 percent of White adults (Sparks et al., 2023). These findings are disturbing, considering that delays in accessing treatment often lead to interacting with the mental health care system in an emergency or crisis, leading to a higher risk of involuntary or forced treatment for minoritized populations (Maura et al., 2017).
Neighborhood and Built Environment
Research on the influence of the neighborhood and built environment such as homes, schools, workplaces, buildings, streets and sidewalks, open spaces, and other infrastructure, including transportation systems on health and health care has grown substantially over the last 20 years (Frehlich et al., 2022; Oakes et al., 2015; Smith et al., 2017). It has clearly been shown that the neighborhood environment is important for health and health behaviors, including birth outcomes, mortality, depression, and early
___________________
7 A non-elderly adult is defined as an individual from 19 to 64 years of age.
child health (Arcaya et al., 2016). However, it has been argued that little insight has been provided into the specific causal processes (Jackson et al., 2009) that can lead to policy solutions. Yet, substantial research has shown that neighborhood disorder and residential segregation by race influences health through a variety of pathways, such as reduced education quality and employment opportunities (Acevedo-Garcia et al., 2008), and is also a fundamental factor influencing racial and ethnic disparities in access to, quality of, and appropriate use of health care services (White et al., 2012).
Social and Community Context
Within the domain of social and community context, one example of a SDOH is food insecurity, defined as being without access to a sufficient quantity of affordable and nutritious food (USDA, 2023a). In 2022, 12.8 percent of U.S. households were food insecure, with 7.7 and 5.1 percent with low or very low food security, respectively. These rates are greater for Black (22.4 percent) and Hispanic (20.8 percent) households, and lower for White (9.3 percent) households (USDA, 2023b). The health impacts of food insecurity affect the entire lifespan, and include obesity (Frongillo and Bernal., 2014), diabetes (Levi et al., 2023), anxiety disorders (Shim and Compton, 2020), and lower life expectancy (Ma et al., 2024). As food insecurity is closely related to poverty, harmful policies help to explain inequities in food insecurity rates among minoritized populations (Shim and Compton, 2020).
Unhealthy food environments, in the form of food deserts and food swamps, are associated with the community context that drives inequitable health outcomes in populations. Food deserts are census tract areas with limited access to healthy and affordable grocery stores (Dutko et al., 2012). Food swamps are saturated with unhealthy food options (e.g., fast food restaurants) (Cooksey-Stowers et al., 2017). People living in unhealthy food environments are at greater risk for poor health outcomes. One study specifically connected poor postoperative outcomes from colorectal cancer with greater odds of living in a food desert or swamp (Khalil et al., 2024).
Health-Related Social Needs (HRSNs)
Deprivation of resources produces poor health and health care outcomes (see discussion on ACEs and life-course associations in Box 2-2). The effects of deprivation manifest as unmet HRSNs,8 which patients in the health care system can experience as financial hardship or financial toxicity,
___________________
8 As defined in chapter 1, HRSNs are social and economic needs that individuals experience that affect their ability to maintain their health and well-being, such as employment, affordable and stable housing, healthy food, personal safety, transportation, and affordable utilities.
BOX 2-2
Life-Course Perspectives on Health Inequities
The life-course perspective suggests that explanations about the causes of inequities in health consider the importance of the timing of exposures across the entire life-span and not just a particular time point. It asserts that various social, biological, and environmental factors over the life-span independently, cumulatively, and interactively impact health in adult life (Lynch and Smith, 2005). Socioeconomic factors affect health throughout life. First, risk factors can affect exposures during gestation, infancy, childhood, adolescence, or adulthood creating a “biological chain of risk.” Second, risk factors can also form a “social chain of risk” that starts with a deprived social environment at the start of life and can set up specific trajectories for health and health care outcomes, particularly chronic diseases, in later life, where the exposures and trajectory of accumulated exposures influence health and health care (Lynch and Smith, 2005). Given that the health status we present to the health care delivery system is impacted by our lives over time, the life-course perspective provides concepts, methods, and theoretical frameworks for guiding our inquiry into how differences in health and need for health care services unfold across our life-span (Halfon et al., 2014).
ACEs include a broad range of traumatic experiences, (e.g., abuse, neglect, and parental separation). ACEs are associated with poorer adult health, including increased high-risk behavior (Hughes et al., 2017). A meta-analysis showed an association between multiple ACEs and many diverse health-related behaviors in adulthood, including physical inactivity, diabetes, smoking, alcohol misuse, poor self-rated health, cancer, heart disease, respiratory disease, substance use disorders, and interpersonal and self-directed violence (Hughes et al., 2017). ACEs are also associated with increased interactions with the juvenile justice system (Graf et al., 2021), and increased delay in medical care due to cost among Black and White adults (Srivastav et al., 2020).
food insecurity, housing insecurity, and transportation needs (Gordon et al., 2020; Mosen et al., 2023). Interventions that address these HRSNs should also consider direct action to eliminate or at least reduce the deprivation that exists across the distribution of SDOH (NASEM, 2019).
This increasingly robust evidence base has led to a growing recognition throughout the health care delivery system that improvement in health and health care outcomes depend at least in part on addressing the social,
Structural racism exposes Black and Brown children to more ACEs via poverty, family disruptions, and community and domestic violence (Mersky et al., 2021; Walsh et al., 2019; Zhang and Monnat, 2022). In early childhood (birth to 11 years), racially and ethnically minoritized children with a lower socioeconomic position had significantly greater odds (4-8 times) of exposure to two or more ACEs compared to White children with higher socioeconomic positions. Notably, socioeconomic position was not protective for minoritized children from higher socioeconomic positions when compared to similarly positioned White children (O’Connor et al., 2020). Chronic stress from the effects of structural racism and other forms of oppression impacts people across the life-span through a process of allostasis, or cumulative wear and tear on the body, and ACEs have been shown to contribute to allostatic load (Finlay et al., 2022). In a landmark study using an index of allostatic load, researchers found that the probability of a high allostatic load increased with age for all groups, with higher allostatic loads among women, people of lower socioeconomic status, and Black people. This phenomenon is known as “weathering” (Geronimus et al., 2006).
Changing demographics are leading to a more diverse older adult population, with significant implications for society, including the need to eliminate health care inequities within this population across the chronic disease continuum (Tucker-Seeley et al., 2021). A framework was introduced for tracking progress and identifying areas of need in health disparities research that recognizes the complex, multifactorial, and multilevel nature of the factors that influence health and health care inequities for older adults (Hill et al., 2015). This framework highlights potential intervention targets across multiple levels of analysis (i.e., biological, behavioral, socio-cultural, and environmental) that are potential facilitators or barriers to health and health care equity across the chronic disease continuum. For example, once inequities are noted either between age groups or across sociodemographic groups among older adults in outcomes of interest, the framework highlights the potential contributing factors that may be altered to help reduce those inequities.
economic, and environmental conditions of communities in which patients live, such as housing status. As a result, health care systems have started to screen for and attempt to address HRSNs that result from exposure to adverse SDOHs. For example, they provide food or to address food insecurity, offer housing resources to address housing insecurity, or cover transportation costs (Castrucci and Auerbach, 2019). While HRSNs focus on interpersonal, individual patient-level interventions, the SDOH generally refer
to more population-level interventions, which deserve equal or greater attention to improve the underlying social and economic conditions that impact whole neighborhoods and communities (Castrucci and Auerbach, 2019).
To better understand the role of the health care delivery system in addressing HRSNs and how such efforts can be integrated into clinical care to achieve more equitable health outcomes, the National Academies released Integrating Social Care into the Delivery of Health Care (NASEM, 2019), which highlighted activities that systems can use. Box 2-3 summarizes
BOX 2-3
Select Recommendations from the 2019 National Academies Report
Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health
Goal 1: Design health care delivery to integrate social care into health care.
Recommendation 1. Health care organizations should take steps to integrate social care into health care. Specific steps include: making and communicating an organizational commitment to addressing health-related social needs and health disparities at the community and individual levels; recognizing that comprehensive health care should include understanding an individual’s social context; and using patient-centered care models to routinely incorporate social risk data into care decisions.
Goal 2: Build a workforce to integrate social care into health care delivery.
Recommendation 2b. Social workers and other social care workers should be considered to be providers who are eligible for reimbursement by payers.
Recommendation 2d. Schools for health professions (including schools of medicine and nursing) as well as continuing education programs should incorporate competency-based curricula on social care. Curricula should include evidence on the social determinants of health, protocols for working in interprofessional teams to address social needs in health care settings, interpersonal and organizational approaches to advancing health equity and decreasing health disparities, and competencies relating to collecting, securing, and using data and technology to facilitate social and health care integration. Schools
examples of recommendations from this report that could advance equity in health care.
Research indicates that interventions to address HRSNs, provided in the appropriate settings and depending on the population, can improve health outcomes and well-being. They may also decrease health care costs (Chuang and Safaeinili, 2023). However, a lack of strategy and coordination and the cost of implementation (Taira et al., 2023) can hinder the effective integration of social needs in health care (NASEM, 2019).
of health professions should also engage social workers in instructional roles in order to model their participation in interprofessional teams and to provide information on social risk screening and social care resources and referrals.
Goal 3: Develop a digital infrastructure that is interoperable between health care and social care organizations.
Recommendation 3f. The parts of the public and private sectors involved in developing and implementing analytic and technology resources, including cell and Internet access, should do so with an explicit focus on equity; the goal should be to avoid unintended consequences such as perpetuation or aggravation of discrimination and bias and the further marginalization of populations and to proceed with an appreciation of the impact on the existing social care system.
Goal 4: Finance the integration of health care and social care.
Recommendation 4b. State Medicaid agencies should use the flexibility described by the Centers for Medicare & Medicaid Services in the social care that Medicaid pays for as a covered service and make the opportunities and limitations associated with that flexibility clear to health plans and health care and social care service providers.
Goal 5: Fund, conduct, and translate research and evaluation on the effectiveness and implementation of social care practices in health care settings.
Recommendation 5b. Funders of health care workforce research (e.g., the Agency for Healthcare Research and Quality and foundations) should include the social care workforce in studies of the effect of the social care workforce on the health and financial outcomes of health care delivery organizations.
NON–HEALTH CARE SECTOR PARTNERSHIPS AND COMMUNITY
Organizations that operate outside of the health care system can take significant steps toward health equity (NASEM, 2017). However, such efforts require commitment, resources (fiscal and human), and partnerships across multiple sectors and at multiple levels: representatives from local and state government, academia, philanthropy, community-based organizations, the health care delivery system, nonprofit policy and advocacy organizations, and the private sector. These non–health care and community-based sectors are not always considered or included when developing health care policies and interventions to reduce inequities (Castillo et al., 2019). Some specific sectors that should be equal partners in collaborative efforts may include housing, education, employment/workforce development, transportation, food/nutrition, social services, and criminal justice.
Intersectoral collaborations to improve health are not new. For example, the “Health in All Policies” approach, where health impacts are considered in policy processes across government agencies, has been developed by multiple governments worldwide (Alderwick et al., 2021).
A number of barriers to intersectoral collaborations to improve population health and achieve health equity exist (Fawcett et al., 2010). First, sectors lack shared responsibility for outcomes. For example, health care providers, insurance companies, employers, and government agencies have competing self- interests in an already fragmented health care system, avoiding a collective responsibility for comprehensively advancing health equity. Second, the health care system lacks effective cooperation and collaboration among players in achieving overall population health goals. Third, no public or private entity is tasked with the overall responsibility for achieving health care equity and optimal health for all. This often contributes to a willingness to proclaim victory for effort rather than meaningful reductions in inequities. Improving overall population health and eliminating health care inequities requires understanding what interventions work and where (i.e., evaluations across various contexts) and a willingness to pay for and sustain such efforts over time (Fawcett et al., 2010).
Coalitions that bring together intersectoral partners can play a substantial role in eliminating health care inequities. This intersectoral approach to coalition building and implementation is necessary to streamline efforts across multiple sectors and multiple health and health care–related issues (Janosky et al., 2013). Success requires a shared frame for envisioning and acting to improve health to ensure identifying the multilevel drivers of health and health care inequities across the life course and the modifiable mechanisms for the coalition to address (Janosky et al., 2013). The work will include identifying specific communities at risk, committing to engaging and listening to members of those communities to identify the root causes
of health inequities and understand local needs and priorities, deciding to make progress on eliminating health inequities, and regularly assessing health outcomes and health inequities (Wong et al., 2015).
Community input and engagement are important in shaping priorities and programs of hospitals and health care systems. Unfortunately, due to systems of oppression described in this chapter, these health care systems often do not equitably value active community input and are not held accountable for diminishing community agency (Petiwala et al., 2021). Many community initiatives, however, lack community voice, support, and participation, all of which are essential for sustainable, long-term change (CDC, 2007; Chouinard et al., 2023). Therefore, establishing innovative avenues for community feedback to foster participation from members, leveraging community strengths, and enhancing existing community assets is needed to ensure culturally sensitive and relevant practices (Ajrouch et al., 2020; NASEM, 2021; Seixas et al., 2020) and sustainability for community-based models and develop a network of community and local agencies (Perez et al., 2016). (See Chapter 6.)
SOCIETAL COMMITMENT TO EQUITY
Little progress can be made to advance equity without a will and commitment to change the status quo. Although many forces threaten the advancement of equity, much support exists for achieving equitable health and health care outcomes for all. Within the health care professional workforce, a commitment to equity is an ethical imperative, as health care professionals have ethical duties of beneficence and nonmaleficence, which include health equity principles (Cyrus and Vinson, 2020). Commitment to health equity partly reflects leaders’ diversity and values. Hospitals with greater representation of racially and ethnically minoritized groups in leadership positions, for example, have greater commitments to diversity initiatives (Herrin et al., 2018). Based on a national survey, approximately half of the hospital boards surveyed reported having no racially or ethnically minoritized board members (Silvera et al., 2023). This commitment extends beyond leadership to medical schools. A study that ranked medical schools by social mission, a measure calculated by assessing the percentage of graduates who work in primary care or health professional shortage areas or are from racial and ethnic backgrounds that are underrepresented in medicine, found that the top three were Historically Black Colleges and Universities: Morehouse School of Medicine, Meharry Medical College, and Howard University (Mullan et al., 2010).
To move society toward a greater commitment to equity, increased public awareness and acceptance of health inequities is needed. One study
found that less than half of the public recognized the influence of social and physical factors on health (Carman et al., 2019). Another found that while large shares of the population believe that some discrimination exist against Black, Hispanic, and Asian people, as many as 40 percent believe in some discrimination against White people (Daniller et al., 2021). It has been well documented that the COVID-19 pandemic disproportionately impacted minoritized populations, yet it did not significantly increase public awareness of racial and ethnic health inequities (Gollust et al., 2020). Nevertheless, all health professionals need greater education on the size and scope of these inequities in health and health care, and effective curricula on health equity should be part of initial education, training, and continuing education in all health professions (Shim and Vinson, 2020). Health equity should become a core competency for all health professionals; curriculum components would include a focus on population health, structural and social determinants of health, and health inequities (Gonzalo et al., 2020).
Greater education about equity will contribute to a greater understanding of the role of external societal forces producing inequities within the health care system. Ultimately, individual members of society need to commit to principles that dismantle structural racism, promote positive SDOH, partner effectively with various communities, and form cross-sector collaborations that center the voices and experiences of minoritized communities (Shim and Vinson, 2020).
Finally, political will is also necessary to advance health equity (Baum et al., 2022). Political climates that support equity and improving outcomes for oppressed and minoritized communities, with the understanding that these interventions can lead to improved health for all communities, are crucial steps toward action. Changing social norms and acting on public health policies can lead to increased political will (Baum et al., 2022). Effective interventions to build political will include greater focus on enhancing opportunity for all and highlighting the interconnectedness of communities (Williams and Cooper, 2019).
CHAPTER SUMMARY
The 2 decades since Unequal Treatment report have seen an increased recognition of the multilevel structural and social determinants of health across the life course and their impact on health care delivery and health outcomes. Structural inequities exist because society has been structured along hierarchical socially assigned racial categories and a group’s location in that hierarchy substantially influences their health, well-being and health care–related outcomes. Structural inequities based on social identity, such as structural racism, have disproportionately allocated negative determinants
of health among racially minoritized populations and the communities in which they live.
Based on the materials in this chapter, the report offers these conclusions.
Conclusion 2.1. The terms used in health and health care equity research have evolved over time and will continue to evolve as further insights are gained and society and demographics shifts.
Conclusion 2.2. Structural determinants of health are the upstream policies and norms that shape the context and creation of social determinants of health and health-related social needs that contribute to the suboptimal health and inequities in the health care system.
Conclusion 2.3. Many of the factors that contribute to racial and ethnic inequities in health care are multilevel and involve societal forces that develop and exist well before individuals enter the health care system.
Conclusion 2.4. Recent advances in the measurement of structural racism have improved the ability to effectively measure the impact of structural racism on health outcomes, strengthening evidence for the significant role of structural racism in driving racial and ethnic health inequities.
Conclusion 2.5. Non–health care sector organizations and community coalitions are critical forces in the elimination of health inequities when valued and engaged as equitable partners and collaborators with health systems.
Conclusion 2.6. Lack of societal commitment to racial and ethnic health equity at multiple levels across the life course has hindered progress to advance health care equity.
REFERENCES
Aaronson, D., D. Hartley, and B. Mazumder. 2021. The effects of the 1930s HOLC “redlining” maps. American Economic Journal: Economic Policy 13(4):355-392.
Abdou, C. M., A. W. Fingerhut, J. S. Jackson, and F. Wheaton. 2016. Healthcare stereotype threat in older adults in the health and retirement study. American Journal of Preventive Medicine 50(2):191-198.
Acevedo-Garcia, D., T. L. Osypuk, N. McArdle, and D. R. Williams. 2008. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Affairs 27(2):321-333.
Adkins-Jackson, P. B., T. Chantarat, Z. D. Bailey, and N. A. Ponce. 2022. Measuring structural racism: A guide for epidemiologists and other health researchers. American Journal of Epidemiology 191(4):539-547.
Ajrouch, K. J., I. E. Vega, T. C. Antonucci, W. Tarraf, N. J. Webster, and L. B. Zahodne. 2020. Partnering with Middle Eastern/Arab American and Latino immigrant communities to increase participation in alzheimer’s disease research. Ethnicity & Disease 30(Suppl 2):765-774.
Alderwick, H., and L. M. Gottlieb. 2019. Meanings and misunderstandings: A social determinants of health lexicon for health care systems. Milbank Quarterly 97(2):407-419.
Alderwick, H., A. Hutchings, A. Briggs, and N. Mays. 2021. The impacts of collaboration between local health care and non-health care organizations and factors shaping how they work: A systematic review of reviews. BMC Public Health 21(1):753.
Alhomsi, A., S. M. Quintero, S. Ponce, I. Mendez, A. L. Stewart, A. M. Napoles, and P. D. Strassle. 2023. Racial/ethnic disparities in financial hardship during the first year of the pandemic. Health Equity 7(1):453-461.
Amiri, S. 2022a. Unemployment and suicide mortality, suicide attempts, and suicide ideation: A meta-analysis. International Journal of Mental Health 51(4):294-318.
Amiri, S. 2022b. Unemployment associated with major depression disorder and depressive symptoms: A systematic review and meta-analysis. International Journal of Occupational Safety and Ergonomics 28(4):2080-2092.
Arastu, A., A. Patel, S. G. Mohile, J. Ciminelli, R. Kaushik, M. Wells, E. Culakova, L. Lei, H. Xu, D. W. Dougherty, M. R. Mohamed, E. Hill, P. Duberstein, M. A. Flannery, C. S. Kamen, C. Pandya, J. L. Berenberg, V. G. Aarne Grossman, Y. Liu, and K. P. Loh. 2020. Assessment of financial toxicity among older adults with advanced cancer. Journal of the American Medical Association Network Open 3(12):2025810.
Arcaya, M. C., R. D. Tucker-Seeley, R. Kim, A. Schnake-Mahl, M. So, and S. Subramanian. 2016. Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Social Science & Medicine 168:16-29.
Bailey, Z. D., N. Krieger, M. Agénor, J. Graves, N. Linos, and M. T. Bassett. 2017. Structural racism and health inequities in the USA: Evidence and interventions. The Lancet 389(10077):1453-1463.
Bailey, Z. D., J. M. Feldman, and M. T. Bassett. 2021. How Structural Racism Works—Racist Policies as a Root Cause of U.S. Racial Health Inequities. New England Journal of Medicine 384(8):768-773.
Barr, D. A. 2014. Health disparities in the United States: Social class, race, ethnicity, and health. Washington, DC: Johns Hopkins Univeristy Press.
Barber, S. 2020. Place matters: From health and health care disparities to equity and liberation. North Carolina Medical Journal 81(3):173-176.
Baum, F., B. Townsend, M. Fisher, K. Browne-Yung, T. Freeman, A. Ziersch, P. Harris, and S. Friel. 2022. Creating political will for action on health equity: Practical lessons for public health policy actors. International Journal of Health Policy and Management 11(7):947.
Blair, I. V., E. P. Havranek, D. W. Price, R. Hanratty, D. L. Fairclough, T. Farley, H. K. Hirsh, and J. F. Steiner. 2013. Assessment of biases against Latinos and African Americans among primary care providers and community members. American Journal of Public Health 103(1):92-98.
Bureau of Labor Statistics. (BLS) 2023. Labor force characteristics by race and ethnicity, 2022. U.S. Department of Labor. https://www.bls.gov/opub/reports/race-and-ethnicity/2022/home.htm (accessed April 29, 2024).
Braveman, P. A., E. Arkin, D. Proctor, T. Kauh, and N. Holm. 2022. Systemic and structural racism: Definitions, examples, health damages, and approaches to dismantling: Study examines definitions, examples, health damages, and dismantling systemic and structural racism. Health Affairs 41(2):171-178.
Brown, T. H., and P. A. Homan. 2022. Frontiers in measuring structural racism and its health effects. Health Services Research 57(3):443.
Bundy, J. D., K. T. Mills, H. He, T. A. LaVeist, K. C. Ferdinand, J. Chen, and J. He. 2023. Social determinants of health and premature death among adults in the USA from 1999 to 2018: A national cohort study. The Lancet Public Health 8(6):e422-e431.
Carman, K. G., S. Weilant, C. Miller, A. Chandra, and M. Tait. 2019. 2018 national survey of health attitudes: Description and top-line summary data. RAND. https://www.rand.org/content/dam/rand/pubs/research_reports/RR2800/RR2876/RAND_RR2876.pdf (accessed April 29, 2024).
Castillo, E. G., R. Ijadi-Maghsoodi, S. Shadravan, E. Moore, M. O. Mensah, M. Docherty, M. G. Aguilera Nunez, N. Barcelo, N. Goodsmith, and L. E. Halpin. 2019. Community interventions to promote mental health and social equity. Current Psychiatry Reports 21:1-14.
Castrucci, B. C., and J. Auerbach. 2019. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Forefront. https://www.healthaffairs.org/content/forefront/meeting-individual-social-needs-falls-short-addressing-social-deter-minants-health (accessed April 29, 2024).
CDC (Centers for Disease Control and Prevention). 2007. Racial and ethnic approaches to community health (reach) U.S.: Finding solutions to health disparities. https://www.cdc.gov/nccdphp/dnpao/state-local-programs/reach/index.htm (accessed March 29, 2024).
Chae, D. H., K. D. Lincoln, N. E. Adler, and S. L. Syme. 2010. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Social Science & Medicine 71(6):1182-1188.
Chae, D. H., A. M. Nuru-Jeter, N. E. Adler, G. H. Brody, J. Lin, E. H. Blackburn, and E. S. Epel. 2014. Discrimination, racial bias, and telomere length in African-American men. American Journal of Preventive Medicine 46(2):103-111.
Chantarat, T., D. C. Van Riper, and R. R. Hardeman. 2021. The intricacy of structural racism measurement: A pilot development of a latent-class multidimensional measure. eClinicalMedicine 40:101092.
Chetty, R., N. Hendren, M. R. Jones, and S. R. Porter. 2020. Race and economic opportunity in the United States: An intergenerational perspective. The Quarterly Journal of Economics 135(2):711-783.
Chouinard, J., T. L. Tovey, and K. Kidd. 2023. The evaluation of equity-focused community coalitions: A review of the empirical literature. Journal of MultiDisciplinary Evaluation 19(45):50-66.
Chuang, E., and N. Safaeinili. 2023. Addressing social needs in clinical settings: Implementation and impact on health care utilization, costs, and integration of care. Annual Review of Public Health 45.
Compton, W. M., J. Gfroerer, K. P. Conway, and M. S. Finger. 2014. Unemployment and substance outcomes in the United States 2002–2010. Drug and Alcohol Dependence 142:350-353.
Cooksey-Stowers, K., M. B. Schwartz, and K. D. Brownell. 2017. Food swamps predict obesity rates better than food deserts in the United States. International Journal of Environmental Research and Public Health 14(11):1366.
Cooper, L. A., D. L. Roter, K. A. Carson, M. C. Beach, J. A. Sabin, A. G. Greenwald, and T. S. Inui. 2012. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health 102(5):979-987.
Crear-Perry, J., R. Correa-de-Araujo, T. Lewis Johnson, M. R. McLemore, E. Neilson, and M. Wallace. 2021. Social and structural determinants of health inequities in maternal health. Journal of Women’s Health 30(2):230-235.
Cutler, D. M., and A. Lleras-Muney. 2006. Education and health: Evaluating theories and evidence. https://www.nber.org/papers/w12352 (accessed April 29, 2024).
Cyrus, K. D., and S. Y. Vinson. 2020. Social justice and advocacy. Social (In) Justice and Mental Health:225. Washington, DC: American Psychiatric Association Publishing.
Daniller, A. 2021. Majorities of americans see at least some discrimination against Black, Hispanic and Asian people in the U.S. Pew Research Center. https://www.pewresearch.org/short-reads/2021/03/18/majorities-of-americans-see-at-least-some-discrimination-against-black-hispanic-and-asian-people-in-the-u-s/ (accessed April 29, 2024).
David, E., T. M. Schroeder, and J. Fernandez. 2019. Internalized racism: A systematic review of the psychological literature on racism’s most insidious consequence. Journal of Social Issues 75(4):1057-1086.
Dickman, S. L., D. U. Himmelstein, and S. Woolhandler. 2017. Inequality and the health-care system in the USA. The Lancet 389(10077):1431-1441.
Devine, P. G., P. S. Forscher, A. J. Austin, and W. T. Cox. 2012. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology 48(6):1267-1278.
Dumas, M. J. 2014. ‘Losing an arm’: Schooling as a site of Black suffering. Race Ethnicity and Education 17(1):1-29.
Duncan-Andrade, J. M. R., and E. Morrell. 2008. The art of critical pedagogy: Possibilities for moving from theory to practice in urban schools. 285. Lausanne, Switzerland: Peter Lang.
Dutko, P., M. Ver Ploeg, and T. Farrigan. 2012. Characteristics and influential factors of food deserts. https://ageconsearch.umn.edu/record/262229/?v=pdf (accessed April 29, 2024).
Estrada, L. V., M. Agarwal, and P. W. Stone. 2021. Racial/ethnic disparities in nursing home end-of-life care: A systematic review. Journal of the American Medical Directors Association 22(2):279-290.e271.
Fawcett, S., J. Schultz, J. Watson-Thompson, M. Fox, and R. Bremby. 2010. Building multisectoral partnerships for population health and health equity. Preventing Chronic Disease 7(6):A118.
Finlay, S., C. Roth, T. Zimsen, T. L. Bridson, Z. Sarnyai, and B. McDermott. 2022. Adverse childhood experiences and allostatic load: A systematic review. Neuroscience & Biobehavioral Reviews 136:104605.
FitzGerald, C., and S. Hurst. 2017. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics 18(1):1-18.
Forde, A. T., D. M. Crookes, S. F. Suglia, and R. T. Demmer. 2019. The weathering hypothesis as an explanation for racial disparities in health: A systematic review. Annals of Epidemiology 33:1-18.e13.
Frank, J., C. Mustard, P. Smith, A. Siddiqi, Y. Cheng, A. Burdorf, and R. Rugulies. 2023. Work as a social determinant of health in high-income countries: Past, present, and future. The Lancet 402(10410):1357-1367.
Frehlich, L., C. D. Christie, P. E. Ronksley, T. C. Turin, P. Doyle-Baker, and G. R. McCormack. 2022. The neighbourhood built environment and health-related fitness: A narrative systematic review. International Journal of Behavioral Nutrition and Physical Activity 19(1):124.
Frongillo, E. A., and J. Bernal. 2014. Understanding the coexistence of food insecurity and obesity. Current Pediatrics Reports 2:284-290.
Fullilove, M. T. 2016. Root shock: How tearing up city neighborhoods hurts America, and what we can do about it. New Village Press: New York, NY.
Furtado, K., N. Rao, M. Payton, K. Brown, R. Balu, and L. Dubay. 2023. Measuring structural racism. https://www.urban.org/research/publication/measuring-structural-racism (accessed April 29, 2024).
Gale, M. M., A. L. Pieterse, D. L. Lee, K. Huynh, S. Powell, and K. Kirkinis. 2020. A meta-analysis of the relationship between internalized racial oppression and health-related outcomes. The Counseling Psychologist 48(4):498-525.
Geronimus, A. T. 1996. Black/White differences in the relationship of maternal age to birthweight: A population-based test of the weathering hypothesis. Social Science & Medicine 42(4):589-597.
Geronimus, A. T., M. Hicken, D. Keene, and J. Bound. 2006. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. American Journal of Public Health 96(5):826-833.
Gollust, S. E., R. I. Vogel, A. Rothman, M. Yzer, E. F. Fowler, and R. H. Nagler. 2020. Americans’ perceptions of disparities in COVID-19 mortality: Results from a nationally-representative survey. Preventive Medicine 141:106278.
Gonzalo, J. D., A. Chang, M. Dekhtyar, S. R. Starr, E. Holmboe, and D. R. Wolpaw. 2020. Health systems science in medical education: Unifying the components to catalyze transformation. Academic Medicine 95(9):1362-1372.
Gordon, N. P., M. P. Banegas, and R. D. Tucker-Seeley. 2020. Racial-ethnic differences in prevalence of social determinants of health and social risks among middle-aged and older adults in a Northern California health plan. PLoS ONE 15(11):e0240822.
Graf, G. H., S. Chihuri, M. Blow, and G. Li. 2021. Adverse childhood experiences and justice system contact: A systematic review. Pediatrics 147(1).
Graham, J. R., L. M. West, J. Martinez, and L. Roemer. 2016. The mediating role of internalized racism in the relationship between racist experiences and anxiety symptoms in a Black American sample. Cultural Diversity and Ethnic Minority Psychology 22(3):369.
Hagiwara, N., F. W. Kron, M. W. Scerbo, and G. S. Watson. 2020. A call for grounding implicit bias training in clinical and translational frameworks. Lancet 395(10234):1457-1460.
Hailu, E. M., S. R. Maddali, J. M. Snowden, S. L. Carmichael, and M. S. Mujahid. 2022. Structural racism and adverse maternal health outcomes: A systematic review. Health & Place 78:102923.
Halfon, N., K. Larson, M. Lu, E. Tullis, and S. Russ. 2014. Lifecourse health development: Past, present and future. Maternal & Child Health Journal 18(2):344-365.
Hardeman, R. R., P. A. Homan, T. Chantarat, B. A. Davis, and T. H. Brown. 2022. Improving the measurement of structural racism to achieve antiracist health policy. Health Affairs 41(2):179-186.
Hatzenbuehler, M. L., S. J. Prins, M. Flake, M. Philbin, M. S. Frazer, D. Hagen, and J. Hirsch. 2017. Immigration policies and mental health morbidity among Latinos: A state-level analysis. Social Science & Medicine 174:169-178.
Herrin, J., K. G. Harris, E. Spatz, D. Cobbs-Lomax, S. Allen, and T. León. 2018. Hospital leadership diversity and strategies to advance health equity. Joint Commission Journal on Quality & Patient Safety 44(9):545-551.
HHS Office of Disease Prevention and Health Promotion. 2024. Social determinants of health. https://health.gov/healthypeople/priority-areas/social-determinants-health (accessed April 29, 2024).
Hill, C. V., E. J. Pérez-Stable, N. A. Anderson, and M. A. Bernard. 2015. The National Institute on Aging health disparities research framework. Ethnicity & Disease 25(3):245-254.
Hill, l. N. Ndugga, and S. Artiga. 2023. Key Data on Health and Health Care by Race and Ethnicity. KFF. https://www.kff.org/racial-equity-and-health-policy/report/key-data-on-health-and-health-care-by-race-and-ethnicity/ (accessed April 29, 2024).
Hill, L., S. Artiga, and A. Damico. 2024. Health Coverage by Race and Ethnicity, 2010–2022. KFF. https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/ (accessed April 29, 2024).
Hoven, H., and J. Siegrist. 2013. Work characteristics, socioeconomic position and health: A systematic review of mediation and moderation effects in prospective studies. Occupational and Environmental Medicine 70(9):663-669.
Hughes, K., M. A. Bellis, K. A. Hardcastle, D. Sethi, A. Butchart, C. Mikton, L. Jones, and M. P. Dunne. 2017. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health 2(8):356-e366.
Isom, J., S. M. Shadravan, and M. Wilson. 2021. Social injustice and substance use disorders Social (in)justice and mental health. Washington, DC: American Psychiatric Association Publishing.
Jackson, L., L. Langille, R. Lyons, J. Hughes, D. Martin, and V. Winstanley. 2009. Does moving from a high-poverty to lower-poverty neighborhood improve mental health? A realist review of ‘moving to opportunity.’ Health & Place 15(4):961-970.
Jemal, A. 2018. Transformative consciousness of health inequities: Oppression is a virus and critical consciousness is the antidote. Journal of Human Rights Social Work 3(4):202-215.
Janosky, J. E., E. M. Armoutliev, A. Benipal, D. Kingsbury, J. L. Teller, K. L. Snyder, and P. Riley. 2013. Coalitions for impacting the health of a community: The Summit County, Ohio, experience. Population Health Management 16(4):246-254.
Kelley, E., E. Moy, D. Stryer, H. Burstin, and C. Clancy. 2005. The national healthcare quality and disparities reports: An overview. Medical Care 43(3 Suppl):I3-8.
Kent, A. H., N. Lanier, D. F. Perkis, and C. James. 2022. Examining racial wealth inequality. Page One Economics.
Khalil, M., M. M. Munir, S. Woldesenbet, Y. Endo, D. I. Tsilimigras, M. F. Kalady, E. Huang, S. Husain, A. Harzman, and T. M. Pawlik. 2024. Association of county-level food deserts and food swamps on postoperative outcomes among patients undergoing colorectal surgery. Journal of Gastrointestinal Surgery 28(4):494-500. https://doi.org/10.1016/j.gassur.2024.01.012.
Kozol, J. 2012. Savage inequalities: Children in America’s Schools. New York, NY: Harper Perennial.
Krieger, N. 2005. Embodiment: A conceptual glossary for epidemiology. Journal of Epidemiology and Community Health 59(5):350.
Krieger, N., R. Kim, J. Feldman, and P. D. Waterman. 2018. Using the index of concentration at the extremes at multiple geographical levels to monitor health inequities in an era of growing spatial social polarization: Massachusetts, USA (2010–14). International Journal of Epidemiology 47(3):788-819.
Lawrence, K., and T. Keleher. 2004. Structural racism. In race and public policy conference. https://www.intergroupresources.com/rc/Definitions%20of%20Racism.pdf (accessed April 29, 2024).
Levi, R., S. N. Bleich, and H. K. Seligman. 2023. Food insecurity and diabetes: Overview of intersections and potential dual solutions. Diabetes Care 46(9):1599-1608.
Lucyk, K., and L. McLaren. 2017. Taking stock of the social determinants of health: A scoping review. PLoS ONE 12(5):0177306.
Lynch, J., and G. D. Smith. 2005. A life course approach to chronic disease epidemiology. Annual Review of Public Health 26:1-35.
Ma, H., X. Wang, X. Li, Y. Heianza, P. T. Katzmarzyk, O. H. Franco, and L. Qi. 2024. Food insecurity and premature mortality and life expectancy in the US. Journal of the American Medical Association Internal Medicine 184(3):301-310.
Matin, B. K., H. J. Williamson, A. K. Karyani, S. Rezaei, M. Soofi, and S. Soltani. 2021. Barriers in access to healthcare for women with disabilities: A systematic review in qualitative studies. BMC Womens Health 21(1):44.
Maura, J., and A. Weisman de Mamani. 2017. Mental health disparities, treatment engagement, and attrition among racial/ethnic minorities with severe mental illness: A review. Journal of Clinical Psychology in Medical Settings 24:187-210.
Mersky, J. P., C. Choi, C. Plummer Lee, and C. E. Janczewski. 2021. Disparities in adverse childhood experiences by race/ethnicity, gender, and economic status: Intersectional analysis of a nationally representative sample. Child Abuse & Neglect 117:105066.
Mosen, D. M., M. P. Banegas, E. M. Keast, and J. F. Dickerson. 2023. Examining the association of social needs with future health care utilization in an older adult population: Which needs are most important? Population Health Management 26(6):413-419.
Mouzon, D. M., and J. S. McLean. 2017. Internalized racism and mental health among African-Americans, US-born Caribbean Blacks, and Foreign-born Caribbean Blacks. Ethnicity & Health 22(1):36-48.
Mullan, F., C. Chen, S. Petterson, G. Kolsky, and M. Spagnola. 2010. The social mission of medical education: Ranking the schools. Annals of Internal Medicine 152(12):804-811.
Mullins, M. A., J. J. Ruterbusch, P. Clarke, S. Uppal, L. P. Wallner, and M. L. Cote. 2021. Trends and racial disparities in aggressive end-of-life care for a national sample of women with ovarian cancer. Cancer 127(13):2229-2237.
Muramatsu, N., and M. H. Chin. 2022. Battling structural racism against Asians in the United States: Call for public health to make the “invisible” visible. Journal of Public Health Management and Practice 28(Supplement 1):S3-S8.
Nardone, A., J. A. Casey, R. Morello-Frosch, M. Mujahid, J. R. Balmes, and N. Thakur. 2020. Associations between historical residential redlining and current age-adjusted rates of emergency department visits due to asthma across eight cities in California: An ecological study. The Lancet Planetary Health 4(1):e24-e31.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2017. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press.
NASEM. 2019. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press.
NASEM. 2021. Implementing high-quality primary care: Rebuilding the foundation of health care. Washington, DC: The National Academies Press.
Netherland, J., and H. Hansen. 2017. White opioids: Pharmaceutical race and the war on drugs that wasn’t. Biosocieties 12(2):217-238.
O’Brien, R., T. Neman, N. Seltzer, L. Evans, and A. Venkataramani. 2020. Structural racism, economic opportunity and racial health disparities: Evidence from US counties. SSM-Population Health 11:100564.
O’Connor, M., N. Slopen, L. Becares, D. Burgner, D. R. Williams, and N. Priest. 2020. Inequalities in the distribution of childhood adversity from birth to 11 years. Academic Pediatrics 20(5):609-618.
Oakes, J. M., K. E. Andrade, I. M. Biyoow, and L. T. Cowan. 2015. Twenty years of neighborhood effect research: An assessment. Current epidemiology reports 2:80-87.
Ortega, A. N., and D. H. Roby. 2021. Ending structural racism in the US health care system to eliminate health care inequities. Journal of the American Medical Aassociation 326(7):613-615.
Paradies, Y. 2006. A systematic review of empirical research on self-reported racism and health. International Journal of Epidemiology 35(4):888-901.
Paradies, Y., J. Ben, N. Denson, A. Elias, N. Priest, A. Pieterse, A. Gupta, M. Kelaher, and G. Gee. 2015. Racism as a determinant of health: A systematic review and meta-analysis. PLoS ONE 10(9):e0138511.
Park, K., and T. C. Yang. 2021. The wealth–health relationship by race/ethnicity: Evidence from a longitudinal perspective. Sociological Forum 36(4):916-938.
Perez, G., P. Della Valle, S. Paraghamian, R. Page, J. Ochoa, F. Palomo, E. Suarez, A. Thrasher, A. N. Tran, and G. Corbie-Smith. 2016. A community-engaged research approach to improve mental health among Latina immigrants: Alma photovoice. Health Promotion Practice 17(3):429-439.
Petiwala, A., D. Lanford, G. Landers, and K. Minyard. 2021. Community voice in cross-sector alignment: Concepts and strategies from a scoping review of the health collaboration literature. BMC Public Health 21:1-11.
Plamondon, K. M., J. L. Bottorff, C. S. Caxaj, and I. D. Graham. 2020. The integration of evidence from the commission on social determinants of health in the field of health equity: A scoping review. Critical Public Health 30(4):415-428.
Powers, B. W., W. H. Shrank, and A. S. Navathe. 2021. Private equity and health care delivery: Value-based payment as a guardrail? Journal of the American Medical Association 326(10):907-908.
Pulok, M. H., K. van Gool, and J. Hall. 2020. Horizontal inequity in the utilisation of healthcare services in Australia. Health Policy 124(11):1263-1271.
Pyke, K. D. 2010. What is internalized racial oppression and why don’t we study it? Acknowledging racism’s hidden injuries. Sociological Perspectives 53(4):551-572.
Rogers, T. N., C. R. Rogers, E. VanSant-Webb, L. Y. Gu, B. Yan, and F. Qeadan. 2020. Racial disparities in COVID-19 mortality among essential workers in the United States. World Medical and Health Policy 12(3):311-327.
Rotter, J., J. C. Spencer, and S. B. Wheeler. 2019. Financial toxicity in advanced and metastatic cancer: Overburdened and underprepared. Journal of Oncology Practice/American Society of Clinical Oncology 15(4):300-307.
Samuel-Ryals, C. A., O. M. Mbah, S. P. Hinton, S. H. Cross, B. B. Reeve, and S. B. Dusetzina. 2021. Evaluating the contribution of patient-provider communication and cancer diagnosis to racial disparities in end-of-life care among medicare beneficiaries. Journal of General Internal Medicine 36(11):3311-3320.
Seixas, A. A., J. Moore, A. Chung, R. Robbins, M. Grandner, A. Rogers, N. J. Williams, and G. Jean-Louis. 2020. Benefits of community-based approaches in assessing and addressing sleep health and sleep-related cardiovascular disease risk: A precision and personalized population health approach. Current Hypertension Reports 22(8).
Sheehy, S., H. J. Aparicio, J. R. Palmer, Y. Cozier, V.-A. Lioutas, J. G. Shulman, and L. Rosenberg. 2023. Perceived interpersonal racism and incident stroke among US Black women. Journal of the American Medical Associoation Network Open 6(11):2343203-2343203.
Shim, R. S., and M. T. Compton. 2020. The social determinants of mental health: Psychiatrists’ roles in addressing discrimination and food insecurity. Focus 18(1):25-30.
Shim, R. S., and S. Y. Vinson. 2020. Social (in)justice and mental health. Washington, DC: American Psychiatric Association Publishing.
Silvera, G. A., C. O. Erwin, and A. N. Garman. 2023. A seat at the table: An examination of hospital governing board diversity, 2011-2021. Journal of Healthcare Management 68(2):132-142.
Slopen, N., T. T. Lewis, and D. R. Williams. 2016. Discrimination and sleep: A systematic review. Sleep Medicine 18:88-95.
Smith, M., J. Hosking, A. Woodward, K. Witten, A. MacMillan, A. Field, P. Baas, and H. Mackie. 2017. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. International Journal of Behavioral Nutrition and Physical Activity 4(1):158.
Sparks, G., A. Montero, A. Kirsinger, I. Valdes, and L. Hamel. 2023. KFF Tracking Poll July 2023: Substance Use Crisis And Accessing Treatment. KFF. https://www.kff.org/other/poll-finding/kff-tracking-poll-july-2023-substance-use-crisis-and-accessing-treatment/ (accessed April 29, 2024).
Srivastav, A., C. L. Richard, C. Kipp, M. Strompolis, and K. White. 2020. Racial/ethnic disparities in health care access are associated with adverse childhood experiences. Journal of Racial & Ethnic Health Disparities 7(6):1225-1233.
Suleman, S., K. D. Garber, and L. Rutkow. 2018. Xenophobia as a determinant of health: An integrative review. Journal of Public Health Policy 39:407-423.
Taira, B. R., K. Yadav, Y. Perez, A. Aleman, L. Steinberg, G. Tchakalian, and R. Tucker-Seeley. 2023. A formative evaluation of social care integration across a safety-net health system. New England Journal of Medicine Catalyst Innovations in Care Delivery 4(4):CAT. 22.0232.
Taylor, L. A., A. X. Tan, C. E. Coyle, C. Ndumele, E. Rogan, M. Canavan, L. A. Curry, and E. H. Bradley. 2016. Leveraging the social determinants of health: What works? PLoS ONE 11(8):0160217.
Trickett, E. J., and S. Beehler. 2013. The ecology of multilevel interventions to reduce social inequalities in health. American Behavioral Scientist 57(8):1227-1246.
Tucker-Seeley, R. D., S. F. Wallington, B. Canin, W. Tang, and J. M. McKoy. 2021. Health equity for older adults with cancer. Journal of Clinical Oncology 39(19):2205-2216.
USDA (United States Department of Agriculture). 2023a. Food security in the U.S.: Measurement. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/measurement/#:~:text=Food%20insecurity%3A%20A%20household%20was,in%20dietary%20quality%20and%20variety (accessed April 29, 2024).
USDA. 2023b. Food security in the U.S.: Key statistics and graphics. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/key-statistics-graphics/#foodsecure (accessed April 29, 2024).
Walsemann, K. M., G. C. Gee, and A. Ro. 2013. Educational attainment in the context of social inequality: New directions for research on education and health. American Behavioral Scientist 57(8):1082-1104.
Walsh, D., G. McCartney, M. Smith, and G. Armour. 2019. Relationship between childhood socioeconomic position and adverse childhood experiences (ACES): A systematic review. Journal of Epidemiology & Community Health 73(12):1087-1093.
Wang, J., M. B. Vela, and M. H. Chin. 2023. Addressing bias and racism against Asian American, Native Hawaiian, and Pacific Islander individuals: A call to action to advance health equity and leadership. Journal of the American Medical Association Network Open 6(7):2325872-2325872.
White, K., J. S. Haas, and D. R. Williams. 2012. Elucidating the role of place in health care disparities: The example of racial/ethnic residential segregation. Health Services Research 47(3 Pt 2):1278-1299.
Wien, S., A. L. Miller, and M. R. Kramer. 2023. Structural racism theory, measurement, and methods: A scoping review. Frontiers in Public Health 11:1069476.
Williams, D. R., and S. A. Mohammed. 2009. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine 32:20-47.
Williams, D. R., J. A. Lawrence, and B. A. Davis. 2019. Racism and health: Evidence and needed research. Annual Review of Public Health 40:105-125.
Williams, D. R., and L. A. Cooper. 2019. Reducing racial inequities in health: Using what we already know to take action. International Journal of Environmental Research and Public Health 16(4):606.
Wong, W. F., T. A. LaVeist, and J. M. Sharfstein. 2015. Achieving health equity by design. Journal of the American Medical Association 313(14):1417-1418.
Wun, C. 2018. Angered: Black and non-Black girls of color at the intersections of violence and school discipline in the United States. Race Ethnicity and Education 21(4):423-437.
Yearby, R., B. Clark, and J. F. Figueroa. 2022. Structural racism in historical and modern US health care policy. Health Affairs (Millwood) 41(2):187-194.
Young, I. M. 2014. Five faces of oppression. Albany: State University of New York.
Zhang, X., and S. M. Monnat. 2022. Racial/ethnic differences in clusters of adverse childhood experiences and associations with adolescent mental health. Social Science and Medicine Population Health 17:100997.
This page intentionally left blank.





























