Breastfeeding in the United States: Strategies to Support Families and Achieve National Goals (2025)
Chapter: Summary
Summary1
In the 2023 Consolidated Appropriations Act, Congress allocated funding for the Department of Health and Human Service’s Office on Women’s Health to contract with the National Academies of Sciences, Engineering, and Medicine (National Academies) to conduct a consensus study on policies, programs, and investments to better understand the landscape of breastfeeding promotion, initiation, and support across the United States; to provide an evidence-based analysis of the macroeconomic, social, and health costs and benefits of the current U.S. breastfeeding rates and goals; and to explore what is known about inequalities in breastfeeding rates and reducing racial, geographic, and income-related breastfeeding variances.
The committee’s statement of task is shown below (Box S-1). To address the full scope of the study, the National Academies convened a committee with expertise spanning lactation and breastfeeding promotion and support, public health, public policy, nursing, nutrition, obstetrics and gynecology, pediatrics, economics, social marketing and public information campaigns related to nutrition, and WIC2 and other public health programs.
Breastfeeding and human milk feeding are the physiological norm for humans and the reference standard for infant feeding and nutrition. The U.S. Surgeon General, as well as prominent organizations of health professionals, have concluded that the short- and long-term health and psychosocial benefits associated with breastfeeding make it a public health
___________________
1 This summary does not include references. Citations for findings presented in the summary as well as Figure S-1 appear in the subsequent chapters of the report.
2 WIC stands for the Special Supplemental Nutrition Program for Women, Infants, and Children.
BOX S-1
Statement of Task
The National Academies of Sciences, Engineering, and Medicine will convene an ad hoc committee of experts to leverage available data and literature to conduct a consensus study on policies, programs, and investments to better understand the landscape of breastfeeding promotion, initiation, and support across the United States. The study will provide an evidence-based analysis of the macroeconomic, social, and health costs and benefits of the United States’ current breastfeeding rates and goals. The study will build on what is known about variances in breastfeeding rates and reducing differences in initiation and continuation. The committee will identify existing gaps in knowledge, areas for needed research, and will discuss challenges in data collection to address said gaps.
Based on available evidence, the committee will address the following issues and offer conclusions and recommendations:
- Best practices for clinicians, healthcare systems, insurers, and employers to encourage breastfeeding by new mothers and to support mothers who are currently breastfeeding, including mothers from populations and those experiencing poverty
- Macroeconomic, health, and social costs of current U.S. breastfeeding rates
- Funding mechanisms, state and federal policies, interventions, and systemic, cross-sector, or field innovations that can support exclusive breastfeeding through the first six months of life
- How insurers implement comprehensive lactation services, set standards to determine reimbursement rates for breastfeeding supplies and services, and provide coverage to help women breastfeed
- Contributing factors that impact breastfeeding rates and access to postpartum maternal care and supportive services (e.g., lactation consultant, doula support, registered dietitians)
- Leverage of available evidence to meet the Healthy People Maternal, Infant, and Child Health breastfeeding goals by 2030.
__________________
NOTE: The project statement of task was revised in April 2024 and June 2025 in response to congressional language and sponsor request.
imperative in the United States. These organizations, along with scientific experts, have determined that for almost all infants, breastfeeding remains the best source of early nutrition and immunological protection, reduces the odds of infant deaths, and is associated with lifesaving protection for preterm infants at risk of developing necrotizing enterocolitis.3 For example,
___________________
3 Necrotizing enterocolitis is the most common serious gastrointestinal disease affecting newborn infants; it typically occurs in the second or third week of life in premature, formula-fed infants. It is characterized by inflammation or death of the tissue of the intestinal lining.
infants who are breastfed “more” versus “less” may have a reduced risk of developing noncommunicable diseases such as asthma, otitis media, obesity in childhood, and childhood leukemia. In addition, a protective association of breastfeeding has been found for infant mortality, including sudden infant death, rapid weight gain and growth, systolic blood pressure, severe respiratory and gastrointestinal infections in younger children, allergic rhinitis, malocclusion, inflammatory bowel disease, and type 1 diabetes. For mothers, health benefits associated with breastfeeding include a reduced risk of developing certain chronic diseases such as breast and ovarian cancer, type 2 diabetes, and hypertension, as well as important psychosocial benefits such as opportunities for emotional bonding.
Previous research has identified that the health benefits of breastfeeding for a mother and her infant or child (i.e., the breastfeeding dyad) can be sustained across the life course and conferred to society at large by avoiding the negative economic cost consequences of suboptimal4 breastfeeding rates. Published models currently estimate the total costs of suboptimal breastfeeding rates in the United States to range from $17.2 billion with an estimated over $100 billion annually.
CURRENT BREASTFEEDING RATES AND NATIONAL GOALS
In the United States, more than 3.5 million women give birth each year, and approximately 84% initiate breastfeeding. Most mothers want to breastfeed, as evidenced by high initiation rates, and the intention5 to breastfeed is a strong predictor of breastfeeding initiation at birth. However, over half of mothers stop breastfeeding earlier than they desire.
Despite high rates of intention and initiation, many mothers and families are unable to meet their own goals as well as national breastfeeding recommendations6 for exclusivity and duration. As shown in Figure S-1, breastfeeding rates decline rapidly between 3- and 12-months postpartum. For example, only 27% of babies receive the U.S. Dietary Guidelines for
___________________
4 To avoid stigmatizing infant feeding decisions or outcomes, this report uses the terms optimal and suboptimal, when possible, to describe breastfeeding rates and highlight that the locus of control extends beyond the breastfeeding dyad or family unit and is impacted by systems-level factors.
5 Breastfeeding intention, as measured in two dimensions by the Infant Feeding Intention scale, qualitatively measures a mother’s intended method of feeding her infant over time (i.e., duration of breastfeeding), as well as the exclusivity of that feeding (e.g., “only breastmilk”).
6 The committee acknowledges that individual breastfeeding goals may differ from national recommendations and that not all mothers choose to or are able to breastfeed exclusively or for extended durations. Many factors may influence infant feeding goals or decisions. National guidelines exist to improve health outcomes over time, not to impose a singular standard of behavior. The committee emphasizes the importance of supporting all families in meeting their own infant feeding goals with dignity and respect.
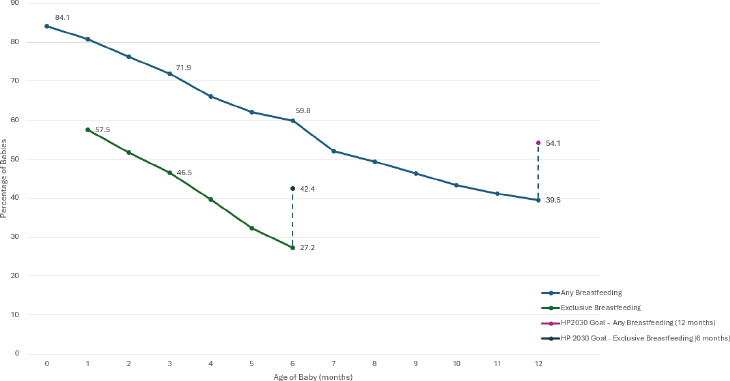
NOTE: The committee chose to use the term human milk throughout the report; however, references to data reflect the terminology used in the original source material. HP2030 = Healthy People 2030.
SOURCE: Adapted from Centers for Disease Control and Prevention, 2022.
Americans (DGA) recommendation for exclusive breastfeeding for the first six months of life. The DGA further recommends introducing appropriate complementary foods at 6 months and continuing breastfeeding through at least 12 months of age. However, fewer than 40% of infants in the United States are still receiving human milk at 12 months.
In alignment with the DGA recommendations, professional and public health organizations recommend that, when possible, breastfeeding be continued with appropriate complementary food for up to two years or longer as mutually desired.
As noted in Figure S-1, these national rates fall short of the Healthy People 2030 goals, which aim for 42.4% of infants to be exclusively breastfed through six months and 54.1% to receive any breastfeeding through 12 months. The sharp decline in breastfeeding after birth highlights persistent challenges for families in meeting their breastfeeding goals, particularly around exclusivity and duration.
Breastfeeding rates are notably lower among certain groups, including Black women, American Indian/Alaska Native women, women with low socioeconomic status, unmarried women, those living in rural areas, and young mothers. Many of these communities of mothers face disproportionate barriers to breastfeeding, such as the need to return to work early, inflexible job conditions, limited access to breastfeeding support services,
and broader cultural and historical challenges. These factors contribute to persistent differences in breastfeeding initiation, duration, and exclusivity.
BREASTFEEDING ACROSS THE LIFE COURSE
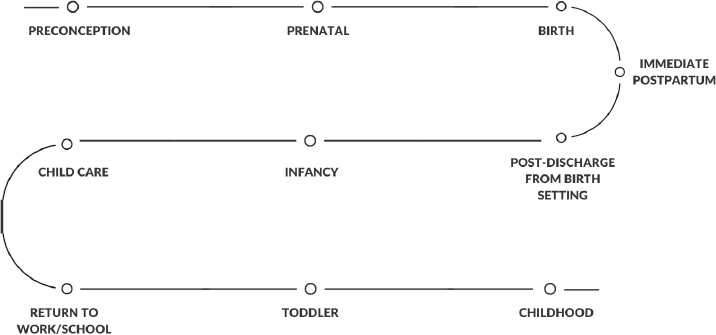
The committee developed this report using a life course framework in recognition that various exposures across different stages of life can influence future chronic disease risk and other health outcomes. This framework identifies multiple determinants (i.e., exposures) that may influence individual and community health, including biological and genetic, behavioral, economic, and social factors. In the case of lactation7 and breastfeeding, an infant and mother’s health trajectories are influenced by exposure to both risk and protective factors, as well as their early life experiences, which can then influence breastfeeding and associated health outcomes at the population level. With this understanding in mind, the committee recognizes that the breastfeeding dyad progresses through a lactation journey, from preconception to birth to postpartum, return to school and work, as well as infancy, amid these intersecting influences. The committee identified critical inflection points across the life course that are specific to human lactation, breastfeeding, and the provision of human milk (Figure S-2).
Human lactation is a multifaceted physiological process that is influenced by a range of factors operating across the life course. The capacity to breastfeed and the outcomes associated with breastfeeding are determined by a combination of biological mechanisms and external factors, including clinical practices, health system structures, and broader social and
___________________
7 Lactation is the physiologic production of human milk; breastfeeding is a dynamic interaction and behavior between a mother and infant.
environmental conditions experienced throughout an individual’s life. The time points illustrated above each represent critical windows in which the foundations for optimal breastfeeding can be laid.
HISTORY OF BREASTFEEDING SUPPORTS IN THE UNITED STATES
Breastfeeding practices and trends in the United States have undergone significant shifts over time. These changes have been influenced by social, cultural, and economic shifts; the growing influence of medicine; and policy and program interventions (Figure S-3)—influences that led to extremely low rates of breastfeeding by the middle of the 20th century. Additional social, cultural, and economic shifts drove a rebounding of breastfeeding rates in later decades, though variances persist across sociodemographic groups.
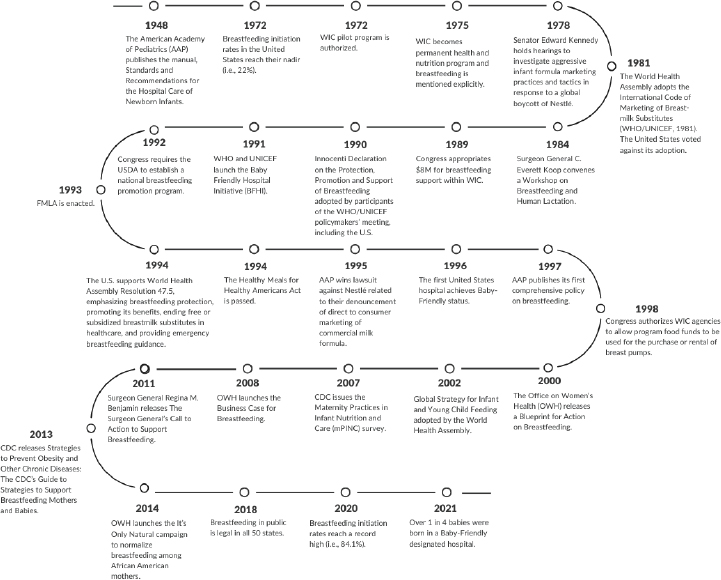
NOTE: CDC = U.S. Centers for Disease Control and Prevention; FMLA = Family and Medical Leave Act; USDA = U.S. Department of Agriculture; WHO = World Health Organization; WIC = Special Supplemental Nutrition Program for Women, Infants, and Children.
While overall breastfeeding rates in the United States have increased over time, notable differences remain across racial, ethnic, geographic, and socioeconomic groups. These patterns reflect both areas of progress and ongoing challenges influenced by a range of historical, cultural, and systemic factors. Addressing these differences calls for a comprehensive approach across settings.
The report’s recommendations explore key actions across settings and topic areas, including community-based settings, public health settings, messaging and the media and marketing environment, health care settings, payment for supplies and services, and workplaces and schools.
THE COMMITTEE’S RECOMMENDATIONS
The means to improve breastfeeding outcomes in the United States, as reflected in the report recommendations below, are multiple and intertwined, and they involve many actors. The committee’s consensus is that central and continuous leadership is necessary to make consistent progress in this area.
In response to its charge and based on the current scientific evidence, the committee presents 16 recommendations to guide the development and implementation of a national breastfeeding strategy across various settings identified in this report. The proposed strategy is organized into five themes:
- Strengthen national coordination efforts
- Expand effective community and public health interventions
- Ensure access to high-quality health care for all
- Adopt and enact breastfeeding-friendly policies to support paid leave and return to work and school
- Invest in research capacity and community-driven approaches
The committee’s recommendations are presented by theme here, numbered by their chapter locations, along with corresponding findings and conclusions.
Strengthen National Coordination Efforts
Multiple government agencies have initiatives and programs to support the breastfeeding dyad, but currently no single entity coordinates the patchwork of government programs into a cohesive road map of supports for the breastfeeding dyad to navigate easily. Coordination and funding across the public health system are limited and insufficient to ensure adequate and culturally competent support for all breastfeeding families.
At the time of this writing, U.S. Department of Health and Human Services has the authority to lead a national breastfeeding strategy and the infrastructure to coordinate efforts among federal, state, tribal, and local partners, as well as the capacity to engage with a diverse range of stakeholders outside of government, including advocacy groups, community organizations, health care systems and providers, employers, and childcare providers. In addition, U.S. Department of Health and Human Services can allocate federal funding to breastfeeding support programs and establish future breastfeeding-friendly policies and initiatives.
Recommendation 4-1: Congress should charge and fund the U.S. Department of Health and Human Services to lead a national breastfeeding strategy, coordinating with federal, state, tribal, and local partners, as well as community groups, health care systems, insurers, workplaces, and academic institutions to ensure that all mothers and families have access to effective and culturally centered breastfeeding support and resources to meet their breastfeeding goals.
Current public health surveillance of breastfeeding indicators provides complementary perspectives on breastfeeding practices, enabling policymakers to identify trends, variances, and areas for intervention. Collecting and analyzing these data over time is critical for identifying trends, addressing variances, and improving and understanding the impact of breastfeeding resources and support. However, current efforts do not adequately capture the wide variety of public health supports for breastfeeding, disaggregated across different demographic groups, that could help identify facilitators and barriers to breastfeeding. Real-time monitoring of breastfeeding trends is also limited; additional attention to real-time changes in breastfeeding rates could help inform the allocation of public health resources and services to communities with the greatest need and further understanding of the effectiveness of existing interventions.
Recommendation 4-2: The U.S. Centers for Disease Control and Prevention should continue to coordinate the surveillance of breastfeeding outcomes and expand the current data collection systems to ensure continuity, coordination, and collaboration across federal, state, tribal, territory, and local programs.
Expand Effective Community and Public Health Interventions
The five recommendations in this section identify ways breastfeeding can be protected, promoted, and supported through expanding effective community and public health interventions. These include supporting
community-led breastfeeding programs and coalitions; ensuring a full complement of breastfeeding support through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program; incorporating infant and young child feeding in emergencies into emergency preparedness and response guidance and plans; implementing public communication strategies for breastfeeding; and regulating the marketing, including labeling and advertising, of commercial milk formula for infant and young child feeding.
Peer groups and social networks, family members, and friends can influence a mother’s decision to breastfeed and her ability to access the support and care she needs to meet her breastfeeding goals. Many promising approaches to supporting breastfeeding are led by community coalitions and peer networks that provide culturally tailored and informed interventions, policy advocacy, and integrated models of care for families. There is strong evidence that peer support (i.e., breastfeeding peer counselors) improves breastfeeding outcomes. This support may be provided by community-led breastfeeding programs or organizations, through existing public health programs (e.g., WIC), or informally in culturally appropriate settings.
Community-led programs and coalitions play a critical role in breastfeeding support, particularly in historically underserved communities. These programs are often developed in response to cultural, social, and structural barriers that may prevent mothers from initiating or sustaining breastfeeding. Many mothers may feel more comfortable receiving breastfeeding guidance from community members who share their background, life experiences, or language. Moreover, community-led initiatives are often embedded within the places where families live, making support accessible and building trust among neighbors.
Recommendation 3-1: Given evidence from burgeoning literature on community-led breastfeeding efforts, Congress; federal, state, and tribal governments; health systems; insurance companies; and philanthropic organizations should fund and establish cross-sector, coordinated investment strategies for supporting community-led breastfeeding programs and coalitions across all local jurisdictions, states, territories, and tribes.
WIC is widely recognized as a highly successful public health nutrition program. Substantial research demonstrates that WIC breastfeeding support, including peer counseling, can increase breastfeeding rates. However, these activities are not standardized across the United States, are not funded to the level needed, and need to be scaled up to adequately meet the needs of all breastfeeding dyads.
Recommendation 4-3: Congress should ensure that the U.S. Department of Agriculture has adequate funding for the Special Supplemental
Nutrition Program for Women, Infants, and Children (WIC), such that every eligible pregnant and postpartum mother in every state, territory, and tribal organization has access to the full complement of WIC breastfeeding support services. This includes (a) adequate base funding for WIC, (b) exploration of the most appropriate funding model (e.g., discretionary vs. mandatory), and (c) expanded funding of the WIC breastfeeding peer counselor program such that all eligible pregnant and postpartum women can receive peer support to meet their breastfeeding goals.
Several factors influence how infant feeding is addressed in public health emergency preparedness, response, and resilience planning. A key challenge is the neglect of infant and young child feeding in these strategies. Humanitarian emergencies, disasters, and other crises often intersect, compounding their impact. However, effective planning and coordination can safeguard infant and child health during emergencies.
Recommendation 4-4: The Federal Emergency Management Agency, state and local emergency management agencies, and nonprofit organizations such as the Red Cross should incorporate infant and young child feeding in emergencies into their emergency preparedness and response guidance and plans. They should share this guidance with states, tribes, territories, and local health jurisdictions and fund efforts that address infant and young child feeding needs during natural disasters and public health emergencies. These actors should collaborate with breastfeeding support organizations in this process, including state, tribal, and community coalitions, as well as offices providing access to the Special Supplemental Nutrition Program for Women, Infants, and Children.
In almost all of the criteria that predict the likelihood of their success, breastfeeding promotion campaigns in the United States face challenges: (a) failure to employ robust social and behavioral change communication frameworks; (b) limited funding and thus limited message exposure; (c) insufficient access to breastfeeding support in health systems and communities; (d) a policy environment that does not provide adequate financial, material, or structural supports for breastfeeding (family leave protections, universal basic income); and (e) a commercial milk formula8 industry that
___________________
8 The term commercial milk formula has been used primarily in the global research context as an umbrella term to describe infant formula, toddler milks, and related products. The term emphasizes that these are commercially produced and marketed products. In the United States, the terms infant formula and toddler milk are most often used to refer to commercially available products.
outspends breastfeeding promotion efforts. A national social and behavioral change communications strategy for promoting breastfeeding can help create an information environment to provide evidence-based information and access to support for breastfeeding.
Recommendation 5-1: The U.S. Department of Health and Human Services, in collaboration with organizations engaged in breastfeeding support at the local, state, and tribal levels, should invest in a multifaceted, coordinated national communication strategy on the importance of breastfeeding and the need for comprehensive support for breastfeeding families from all of society across the lactation journey.
- The strategy should consider the full range of audiences: (a) women who may breastfeed; (b) their partners and family members; (c) community members and community organizations; (d) health care providers, health systems, pharmacies, health professional societies, and insurers; (e) business leaders and a wide range of employers, including childcare centers, schools, transportation agencies, the military, and the criminal justice system; (f) public health systems and authorities; and (g) policymakers at the federal, state, tribal, and local levels.
- The strategy should apply established social and behavior change communication frameworks and ensure that all stages of campaign development involve members of impacted communities, including historically underserved populations.
- The strategy should also include information about what resources are available and where and how to access them (e.g., in the health care setting, in community and public health settings, payment requirements for services and supplies).
The committee reviewed previously published studies and reviews on the impact of commercial milk formula marketing on breastfeeding-related attitudes, norms, and behaviors. Studies consistently show that exposure to commercial milk formula marketing through diverse media channels, including digital and social media spaces, influences infant feeding perceptions, attitudes, and practices.
Recommendation 5-2: The U.S. Food and Drug Administration and U.S. Federal Trade Commission should coordinate to rigorously regulate the marketing, including labeling and advertising, of commercial milk formula for infant and young child feeding, informed by the principles outlined in The International Code of Marketing of Breast-Milk Substitutes, across media, retail, health care, and other settings.
Ensure Access to High-Quality Care for All
Throughout its deliberations, the committee found that the current system of breastfeeding and lactation support is fragmented and uncoordinated; it does not provide standard and optimal care for the breastfeeding dyad. For example, in the health care setting, there is no “medical home” (i.e., single health care setting) for the breastfeeding dyad, which consistently presents challenges in the continuity of maternal and pediatric care and in insurance payment for breastfeeding services and human milk supplies. In addition, the health care system struggles to provide timely delivery and coordination of lactation-related care and resources that are mandated by law, as is the case with insurance payment for lactation support services and medical supplies.
The following recommendations describe the importance of maternity care practices, investment in the lactation support workforce, development of health care performance measures, extension of postpartum Medicaid coverage for low-income women, and comprehensive coverage and payment for breastfeeding services and supplies.
The Baby-Friendly Hospital Initiative (BFHI) is a well-established, evidence-based program designed to improve breastfeeding outcomes. The program, launched by United Nations Children’s Fund (UNICEF) and the World Health Organization, aligns maternity and newborn care practices with the Ten Steps to Successful Breastfeeding. Since its inception, the BFHI has demonstrated consistent and substantial benefits for breastfeeding initiation, exclusivity, and duration across a variety of health care settings. In the United States, implementation of the Ten Steps, whether through formal Baby-Friendly designation or through stepwise policy adoption, has been associated with improved outcomes and reductions in breastfeeding disparities, especially when community engagement and culturally responsive practices are centered.
Recommendation 6-1: The U.S. Centers for Medicare & Medicaid Services and The Joint Commission, in collaboration with other hospital accrediting bodies, hospital associations, and state health regulators, should ensure that every maternity care facility in the United States implements the UNICEF/World Health Organization’s Baby-Friendly Hospital Initiative’s Ten Steps to Successful Breastfeeding as the standard of care.
Accrediting or regulatory bodies for health professionals, including state licensing boards for nursing, could explore including a minimum set of competencies in human lactation and breastfeeding into their licensing, certification, and accreditation requirements. This could ensure that individuals providing breastfeeding support in health care settings would have a shared, minimum level of training and education.
In addition, a significant portion of the lactation support workforce is employed in community-based or public health settings, such as the WIC program. Thus, federal and state investment in education and training initiatives for registered dietitians, nutritionists or nutrition assistants, providers with the International Board Certified Lactation Consultant® (IBCLCs) designation, and breastfeeding peer counselors is critical to ensure that community-level needs are met for primary breastfeeding care. In addition, investment in these initiatives could support data collection on workforce capacity and compensation to ensure that lactation support providers from historically underserved communities are compensated for their work appropriately.
The current lactation support workforce in the health care setting consists of a wide range of providers (e.g., nurses and nurse practitioners, midwives, physicians, advanced practice professionals, IBCLCs, registered dietitians, peer counselors, and doulas). Their education and training differ widely with respect to breastfeeding care and training.
Recommendation 6-2: Accrediting boards and regulatory bodies for health professionals, federal and state agencies, public health organizations, and philanthropic organizations should increase investment in the training and availability of lactation support providers.
- Accrediting and regulatory bodies for health professionals and state boards of nursing should include a minimum set of competencies in human lactation and breastfeeding into their licensing, certification, and accreditation requirements.
- Federal agencies, such as the U.S. Health Resources and Services Administration and U.S. Department of Agriculture, in collaboration with state, tribal, and local governments, should work together to provide support for the training and certification of health professionals or lactation support providers to provide breastfeeding support services (e.g., through the breastfeeding peer counseling program offered by the Special Supplemental Nutrition Program for Women, Infants, and Children).
- Public health organizations and philanthropic organizations should work together to fund initiatives to increase the number of lactation support providers to ensure that their communities’ lactation needs are met.
A Healthcare Effectiveness Data Information Set (HEDIS) is a widely used tool for measuring health care performance used by over 90% of U.S. health plans, covering more than 190 million enrollees. The creation of a HEDIS performance measure for breastfeeding would require creating
automated fields in electronic health records to better capture infant feeding practices across time (i.e., in the birth setting and during postpartum and pediatric care). Practices at baseline and after implementing improvement projects could be recorded to assess how well health plans and health care providers protect, support, and promote breastfeeding. In addition, measures that are aligned with the care and support of sick or vulnerable infants could be established to better track breastfeeding outcomes and future investment in inpatient settings.
Recommendation 6-3: The U.S. Centers for Medicare & Medicaid Services should develop and implement a Healthcare Effectiveness Data Information Set performance measure of breastfeeding.
Medicaid expansion has positively influenced breastfeeding rates by increasing access to prenatal education, postpartum lactation support, breast pumps, and maternal health care. The extension of postpartum Medicaid coverage from 60 days to 12 months is particularly promising, as it can help mothers with low incomes sustain breastfeeding beyond the initial few weeks postpartum. By reducing variances in access to critical services, Medicaid expansion and extension efforts not only improve maternal and infant health outcomes but also may promote higher breastfeeding initiation and duration rates among low-income populations.
Recommendation 7-1: The U.S. Centers for Medicare & Medicaid Services should continue to ensure that postpartum Medicaid extension is available to all eligible pregnant and postpartum women up to 12 months after birth, at a minimum; all states should implement this option.
Currently, coverage or payment for breastfeeding care in the United States is complex and often opaque to families needing support. Navigating this complex system can be difficult for a new family, and breastfeeding care is fragmented between parallel systems that provide separate appointments and services to a mother and her infant or child. Health insurance coverage for families is critical, as it ensures that mothers and their children have access to essential medical care, and this coverage before and during pregnancy and postpartum can help prevent birth complications, support breastfeeding, and provide essential newborn care, all of which set a strong foundation for lifelong health. Inconsistencies in insurance coverage can hinder mothers from receiving standard, high-quality, and timely health care, which can affect breastfeeding initiation and duration rates. Clear guidelines, uniform enforcement of coverage requirements,
and communication between health care providers, insurers, and members of the public could all help to address these inconsistencies to ensure that all mothers have equal access to essential lactation support services and supplies.
Recommendation 7-2: The Centers for Medicare & Medicaid Services and the Federal Insurance Office, in collaboration with public and private payers, should create and ensure comprehensive coverage and payment of breastfeeding services and supplies to guarantee equal access to a standard package of services and durable medical equipment.
Adopt and Enact Breastfeeding-Friendly Policies to Support Leave and Return to Work and School
Returning to work or school poses a major challenge for breastfeeding mothers, as consistent infant and mother contact is important for sustaining breastfeeding. Working mothers encounter distinct challenges in sustaining breastfeeding, and these experiences vary from person to person. The recommendations that follow are focused on paid family and medical leave for working families and the enforcement of lactation protections in the workplace and schools.
There is consistent causal evidence that state mandates providing 12 weeks of paid family leave have positive effects on the duration of breastfeeding. Therefore, 12 weeks should be the minimum threshold for a federal paid family leave policy. Moreover, compelling evidence from Canada suggests that providing longer periods of paid family leave will generate even more increases in breastfeeding duration. Consistent with the scientific consensus on the health benefits of exclusive breastfeeding for the first six months postpartum, a number of studies find that paid family leave policies of up to six months in other high-income countries confer health benefits to mothers and infants.
Recommendation 8-1: Congress should enact national paid family and medical leave for all postpartum mothers. In the absence of a national plan, states and employers should enact this coverage.
Several laws protect lactation accommodations for employees and students in the United States, but enforcement mechanisms vary across workplaces and educational institutions. While federal laws establish baseline protections, they could be further strengthened to support breastfeeding. Additionally, enforcement depends largely on complaints, legal action, and oversight by government agencies.
Recommendation 8-2: Federal, state, territorial, tribal, and local governments, in collaboration with the public and private sectors, should (a) strengthen and enforce existing laws and legislation that guarantee that lactation accommodations and spaces are available in all workplaces, schools, colleges, universities, and childcare centers and (b) ensure that they comply with federal and state legal requirements.
Invest in Research Capacity and Community-Driven Approaches
The committee identified that conducting innovative breastfeeding research requires a range of investments to ensure high-quality, impactful studies. This may include cost-benefit analysis of interventions. These investments span financial resources, infrastructure, workforce development, policy support, and technology integration, as described in two recommendations.
Recommendation 9-1: The National Institutes of Health, along with other federal and nonfederal agencies, should expand funding and prioritize key breastfeeding research and implementation questions geared toward scaling up supports to achieve the Healthy People 2030 infant feeding goals.
Recommendation 9-2: The National Institutes of Health should develop an action plan for prioritizing community, clinical, and translational breastfeeding research across its institutes and centers; this plan should build on existing initiatives.
Conclusion
The recommendations presented in this report present proven overall strategies across multiple settings for supporting all families on their lactation journeys. They outline approaches that will foster the conditions and systems needed to achieve national goals to increase overall breastfeeding rates and address variances in these rates and health outcomes across populations.















