A Long COVID Definition: A Chronic, Systemic Disease State with Profound Consequences (2024)
Chapter: Summary
Summary1
Individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), can experience ongoing symptoms after acute infection. This complex and lingering disease state known as Long COVID has profound medical, social, and economic consequences worldwide. Long COVID prevalence estimates vary widely, and some estimates of the percentage of those infected with COVID-19 who develop Long COVID range from 10 to 35 percent or higher. For example, a U.S. Census Bureau and the National Center for Health Statistics Household Pulse Survey showed, as of March 5 to April 1, 2024, about 17.6 percent of all U.S. adults have “ever experienced with Long COVID” and 6.9 percent of all U.S. adults are “currently experiencing Long COVID.”2
Several working definitions that describe Long COVID exist currently. However, no common definition for Long COVID has yet been agreed upon. In August 2022, the Office of the Assistant Secretary for Health (OASH) published an interim working definition for Long COVID based on collaboration among several government agencies and outside subject matter experts, including medical societies and patients. Other major health organizations in the United States and internationally have also published various definitions of Long COVID and related terms. Furthermore,
___________________
1 This summary does not include references. Citations for the discussion presented in the summary appear in the subsequent report chapters.
2 The Pulse Survey defined Long COVID as “any symptoms lasting 3 months or longer that [they] did not have prior to having coronavirus or COVID-19.”
several journal articles have proposed different ways in which Long COVID could be defined. The lack of a consensus definition presents challenges for patients, clinicians, public health practitioners, researchers, and policy makers. The diversity of Long COVID patient presentations, the overlap with other conditions, and the difficulty of ascribing symptoms to an earlier infection make defining Long COVID particularly challenging. For patients, challenges associated with the diversity of clinical presentations that can accompany a diagnosis of Long COVID may lead to difficulties accessing medical care and obtaining support; skepticism and dismissal of their experiences by medical professionals, peers, family members, and employers; delayed or denied treatment; and social stigma.
Recognizing the need for broad input and careful consideration of an improved definition, the Administration for Strategic Preparedness and Response (ASPR) and OASH asked the National Academies of Sciences, Engineering and Medicine (National Academies) Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats to take up the issue of defining Long COVID. To accomplish this complex task, a separate
BOX S-1
2024 NASEM Long COVID Definition
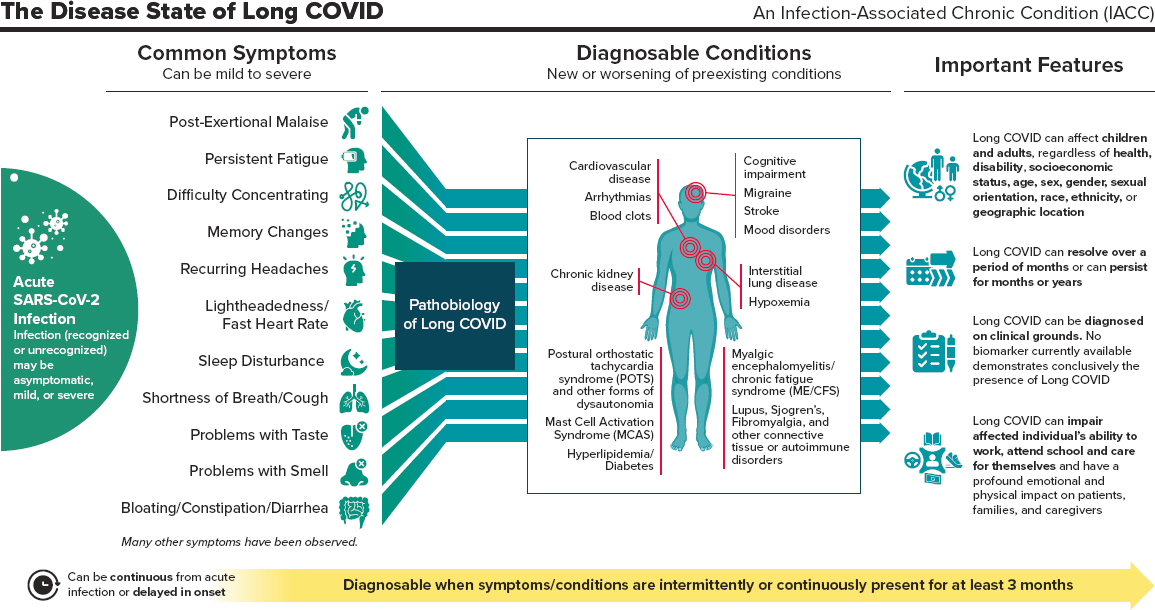
Long COVID (LC) is an infection-associated chronic condition (IACC) that occurs after SARS-CoV-2 infection and is present for at least 3 months as a continuous, relapsing and remitting, or progressive disease state that affects one or more organ systems.
LC manifests in multiple ways. A complete enumeration of possible signs, symptoms, and diagnosable conditions of LC would have hundreds of entries. Any organ system can be involved, and LC patients can present with
- single or multiple symptoms, such as shortness of breath, cough, persistent fatigue, post-exertional malaise, difficulty concentrating, memory changes, recurring headache, lightheadedness, fast heart rate, sleep disturbance, problems with taste or smell, bloating, constipation, and diarrhea.
- single or multiple diagnosable conditions, such as interstitial lung disease and hypoxemia, cardiovascular disease and arrhythmias, cognitive impairment, mood disorders, anxiety, migraine, stroke, blood clots, chronic kidney disease, postural orthostatic tachycardia syndrome (POTS) and other forms of dysautonomia, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), mast cell activation syndrome (MCAS), fibromyalgia, connective tissue diseases,
expert committee, the Committee on Examining the Working Definition of Long COVID, was established. The committee consisted of experts in the fields of health research and policy, research related to Long COVID and chronic multi-symptom illness, clinical practice and guidelines, infectious diseases, public health and epidemiology practice, social and behavioral sciences, patients and lived experience, and community engagement and health equity.
To define Long COVID, the committee employed a systematic approach implemented through a multi-phase process with activities engaging more than 1,300 participants, with a focus on the patient perspective and interdisciplinary dialogue. The committee also assembled and analyzed reviews and primary literature on Long COVID and examined existing Long COVID definitions. In developing the definition, the committee considered the following criteria: precision, feasibility, acceptability, accessibility, balancing benefits and harms, potential impact on health equity, and unintended consequences.
- hyperlipidemia, diabetes, and autoimmune disorders such as lupus, rheumatoid arthritis, and Sjogren’s syndrome.
Important Features of LC:
- LC can follow asymptomatic, mild, or severe SARS-CoV-2 infection. Previous infections may have been recognized or unrecognized.
- LC can be continuous from the time of acute SARS-CoV-2 infection or can be delayed in onset for weeks or months following what had appeared to be full recovery from acute infection.
- LC can affect children and adults, regardless of health, disability, or socioeconomic status, age, sex, gender, sexual orientation, race, ethnicity, or geographic location.
- LC can exacerbate pre-existing health conditions or present as new conditions.
- LC can range from mild to severe. It can resolve over a period of months or can persist for months or years.
- LC can be diagnosed on clinical grounds. No biomarker currently available demonstrates conclusively the presence of LC.
- LC can impair individuals’ ability to work, attend school, take care of family, and care for themselves. It can have a profound emotional and physical impact on patients and their families and caregivers.
2024 NASEM LONG COVID DEFINITION
Relying on findings reported in the literature as well as input from engagement activities, the committee proposes the 2024 NASEM Long COVID Definition (see Box S-1 and Figure S-1). The 2024 NASEM Long COVID Definition consists of a core component in bold font, plus a set of illustrative symptoms and diagnosable conditions, followed by seven important features that elaborate on the core component. The committee chose to put forth a single definition for Long COVID. This definition is intended to cover most, if not all patients who experience Long COVID. The committee recognizes that eligible subsets who fit within the overall definition would need to be specified for particular purposes, such as research or surveillance.
The committee intends its definition to be applied to many purposes. These may include clinical care and diagnosis; eligibility for health services, insurance coverage, disability benefits, and school or workplace accommodations; public health; social services; policy making; epidemiology and surveillance; private and public research; and public awareness and education, especially for patients and their families and caregivers. In all these situations, the committee intends its Long COVID definition to interface with existing practices and policies without worsening health disparities or other problems.
In its report, the committee specifically offers ways in which the 2024 NASEM Long COVID Definition may be applied for clinical, research, and public health surveillance purposes and provides considerations as well as illustrative examples. Furthermore, the committee believes all stakeholders involved in social safety net programs, including but not limited to payers, workplaces and employers, academic institutions and educators, and support services and government, need to be aware of Long COVID to properly support patients, and their families and caregivers in need. In this regard, the committee refers the reader to the National Academies report, Long-Term Health Effects Stemming from COVID-19 and Implications for Social Security Administration.
The committee hopes that the 2024 NASEM Long COVID Definition will aid clinicians in the consistent diagnosis, documentation, and treatment of Long COVID; encourage further research into the pathophysiology, diagnosis, prognosis, consequences, and treatment of Long COVID; enhance patient access to appropriate care, treatment, services, and benefits; and harmonize research and surveillance efforts on Long COVID, while providing researchers flexibility in the design of studies on Long COVID; and raise awareness and educate the public about Long COVID.
KEY ELEMENTS OF THE DEFINITION
The committee found no published, standardized guidelines for developing disease definitions. The committee gleaned lessons from the process of developing disease definitions for other multi-symptom conditions and took advantage of existing definitions for Long COVID, adopting elements when appropriate. The committee articulated several possible key elements of a disease definition: attribution, time, clinical features, equity, functional impairment, exclusions and alternative diagnoses, biomarkers and laboratory criteria, and risk factors. Below is a description of how the committee approached each key element of the definition.
The 2024 NASEM Long COVID Definition includes a few notable features and specifically introduces a few new features that existing definitions lack. It provides explicit examples of common symptoms and conditions that are characteristic of Long COVID. The definition requires symptoms or conditions to be present for a duration of 3 months or more. Notably, while symptoms need to be present for at least 3 months, the timing of those 3 months is unspecified. The definition also firmly acknowledges the profound impact of Long COVID on function and the ability of patients to work, attend school, take care of family, and care of themselves. The new definition also introduces an equity statement—“Long COVID can affect children and adults, regardless of health, disability, or socioeconomic status, age, sex, gender, or sexual orientation, race, ethnicity, or geographic location”—recognizing that social determinants and structural inequalities intersect to create health disparities and to discourage stereotypical assumptions and biases that could deflect patients, clinicians, public health practitioners, researchers, and policy makers from recognizing all those who experience Long COVID. The definition does not require laboratory confirmation or other proof of initial SARS-CoV-2 infection, recognizing that the initial infection may or may not have been recognized due to various factors, including the lack of availability of and limited access to tests early in the pandemic, limited sensitivity of some SARS-CoV-2 tests and the potential for false negatives, as well as financial barriers to testing even when tests were more widely available.
Terminology Considerations
Using consistent terminology is as important as using a consistent definition. In medicine, the word “illness” often refers to the “innately human experience of symptoms and suffering,” while the term “disease” often refers to an “alteration in biological structure or functioning.” To stress the systemic reality of Long COVID, while acknowledging uncertainty about etiology, this report adopts the term “disease state” when referring to Long COVID. In addition to using “disease state” when referring to Long COVID,
the committee uses the terms “condition,” “medical condition,” or “chronic condition.” Similarly, when referring to the unhealthy state related to any prior infection, the committee uses the term “infection-associated chronic condition.” The term “infection-associated chronic condition” (IACC) applies to a variety of chronic conditions that can be triggered by viruses, bacteria, fungi, or parasites. Use of this term highlights the ongoing nature of the medical condition and its association with a triggering infection without conveying any unwarranted conclusions about pathobiological mechanisms.
Over the course of the COVID-19 pandemic, various terms have been applied to what this report terms “Long COVID.” These include “long-haul COVID,” “post-COVID conditions,” “post-COVID syndrome,” “postacute COVID-19 syndrome,” “chronic COVID,” and “post-acute sequelae of SARS-CoV-2 infection (PASC).” All these terms pertain to the same broad clinical condition. The committee intentionally adopted the patient-developed term “Long COVID” because its simplicity and familiarity can facilitate communication within and between the scientific community and the public. Long COVID is also consistent with World Health Organization recommendations to adopt unbiased, neutral, non-stigmatizing descriptive terms when the cause, mechanism, or pathology of a new condition have not yet been established.
Attribution to Infection
The 2024 NASEM Long COVID Definition states that Long COVID occurs after acute SARS-CoV-2 infection but does not require laboratory confirmation or other proof of initial infection. The definition emphasizes that Long COVID can follow infections of any severity (including asymptomatic infections), whether they were initially recognized or not. Because no test for SARS-CoV-2 infection has perfect sensitivity and because the rates of false negatives from antigen and PCR tests vary with time and other factors, some infected individuals will receive negative test results. Antibody testing can sometimes indicate a past SARS-CoV-2 infection, but antibody levels can fluctuate or wane over time. Vaccination against COVID-19 also complicates antibody testing as it can cause positive results on some antibody tests. Additionally, some individuals were not tested or could not access testing during a suspected acute SARS-CoV-2 infection. Individuals experiencing an asymptomatic infection may not be tested for SARS-CoV-2, yet a variety of post-acute sequelae can occur after asymptomatic or mild infections.
Onset and Duration
The 2024 NASEM Long COVID Definition specifies 3 months as the minimum duration of symptoms, which means that 3 months after infection, whether consistent or relapsing and remitting, is the earliest that symptoms can be designated as Long COVID. Although the definition specifies a minimum duration of 3 months to qualify as Long COVID, a clinician should recognize, acknowledge, and monitor concerning symptoms before the 3-month mark. These symptoms should be assessed and treated appropriately, and the ICD-10 code U09.9 (post COVID-19 condition, unspecified) may be used even before establishing a Long COVID diagnosis. Most patients with acute SARS-CoV-2 infection recover after a period of days to weeks. A 3-month cutoff will likely provide enough time for most patients to recover from acute manifestations of COVID-19. The choice of a 3-month minimum duration may allow for the resolution of temporary symptoms that are due to non-medical circumstances (e.g., overwork, stressful situations, medication side effects) and may allow for evaluation and treatment for alternative conditions with similar initial presentations.
Because there is still ambiguity regarding the relationship between the timing of SARS-CoV-2 infection relative to Long COVID onset, the committee chose not to include a maximum latency period. Although this action may lead to an increase in the number of people diagnosed with Long COVID, any maximum latency chosen would be speculation without the backing of scientific evidence. Furthermore, such a move might exclude people who develop delayed onset Long COVID, did not recognize they might be affected by Long COVID until later in its course, or were not able to access care due to the availability or restrictive criteria of some Long COVID clinics.
At the same time, none of the symptoms or conditions associated with Long COVID are unique to that condition. As the number of cases of acute SARS-CoV-2 infection declines, an increasing fraction of patients with symptoms compatible with Long COVID will have their condition due to a different origin. The report suggests that by 2025, it will be prudent for the clinician considering a diagnosis of Long COVID to seek evidence of prior acute SARS-CoV-2 infection. Over time, if and as the time horizon for Long COVID following acute infection becomes more sharply defined, this will be an important aid to clinical judgment.
Symptoms, Temporal Pattern and Duration of Symptoms, and Symptom Severity
The 2024 NASEM Long COVID Definition does not list any symptoms or conditions as being required and does not list any symptoms or
conditions as being exclusionary; this may have the effect of lessening the specificity while increasing the sensitivity of the diagnosis. The committee offered some examples of how Long COVID could manifest, including some symptoms and conditions, and how Long COVID could present as a new condition or an exacerbation of pre-existing conditions. This list is not meant to be exhaustive or to dismiss the significance of other symptoms or conditions. Studies estimate the prevalence of over 200 symptoms in multiple organ systems, and these symptoms can occur at varying frequencies. Another notable feature of Long COVID is the variable temporal pattern and duration of symptoms. The committee also recognizes that the severity of Long COVID symptoms can range from mild to severe.
Equity
Equity needs to be considered at multiple steps in a Long COVID patient’s journey to obtain care and services. Findings from the engagement process emphasized the need to address equity in the definition, with one participant saying, “It could be helpful to include a specific statement around health equity in a Long COVID definition. That would maybe be a little unusual to include in a definition, but it is important, if not in the definition, somewhere else.” The 2024 NASEM Long COVID Definition acknowledges that a Long COVID diagnosis may be considered regardless of health status, vaccination history, or demographics. This definition applies to both adult and pediatric patients. Socioeconomic factors, inequality, discrimination (based on race and gender, among others), bias, and stigma affect whether patients can receive a diagnosis and benefit from Long COVID-targeted health care or services. These factors include but are not limited to access to COVID-19 testing during acute illness, access to evaluation for possible Long COVID, willingness of physicians to diagnose a particular patient, access to insurance benefits, and patients’ fears of stigmatization that could result from having a Long COVID diagnosis. No existing Long COVID definitions include references to equity.
Functional Impairment
The 2024 NASEM Long COVID Definition emphasizes that some individuals with Long COVID are severely affected and can have a variety of activity limitations. This can profoundly affect patients’ and caregivers’ lives and is an important feature of Long COVID. In the evidence review, the committee found publications documenting a range of mild to severe functional impairments, activity limitations, and quality of life impacts in individuals with Long COVID.
Alternative Diagnosis, Biomarkers, and Risk Factors
Consideration of alternative diagnoses is not directly addressed in the 2024 NASEM Long COVID Definition, and risk factors are not included. As an important consideration, the definition notes that no definitive biomarkers currently exist to determine the presence of Long COVID. The committee elected not to include a statement regarding exclusions or alternative diagnoses in the 2024 NASEM Long COVID Definition. There is no scientific evidence that any medical condition precludes the diagnose of or cannot exist alongside Long COVID. The 2024 NASEM Long COVID Definition does note myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS), among others, as examples of diagnosable conditions that can be part of the picture of Long COVID. These and other potentially overlapping conditions are compatible with a diagnosis of Long COVID. While risk factors, such as underlying comorbid conditions, may influence the probability and presentation of COVID-19 and of Long COVID, the proposed definition does not directly consider the potential for differential risk according to patient characteristics.
A WORKING DEFINITION AND RESEARCH AGENDA
The committee believes that the 2024 NASEM Long COVID Definition should be revised as new evidence emerges and our understanding of Long COVID continues to evolve. This is in line with lessons from defining other diseases such as HIV/AIDS, which took years and multiple iterations to refine. Given the current pace of research, it is possible that the definition may need to be updated in no more than 3 years’ time and will continue to require a multidisciplinary effort. Other triggers for updating the 2024 NASEM Long COVID Definition could include the emergence of new treatments with clear benefits for patients identified as a subset of people with Long COVID, the development of a new test, new evidence on prognosis, or other opportunities to improve the clarity or precision of the definition.
Looking ahead, it may also be valuable to have mechanisms in place for gauging how the 2024 NASEM Long COVID Definition is understood, how it is being used, what other elements need to be added, and whether it is being applied in a consistent and standardized way (e.g., assessment tools). A research agenda centered around improving the definition could focus on the key definition elements articulated in the report: attribution to infection, time, clinical features, equity, functional impairment, exclusions and alternative diagnoses, biomarkers and laboratory criteria, and risk factors.
New evidence of the following may play a role in decisions to reconsider the definition:
- Improved testing to identify those who have been infected, even when tested weeks, months and years later. However, a large proportion of the population has been infected with COVID-19 at this point, and, as a result, finding uninfected control groups will become an increasing challenge in conducting research.
- Symptoms and organ damage that distinguish Long COVID from healthy people and other medical conditions.
- Onset and duration, including delayed onset of Long COVID after an ostensible period of recovery from acute infection.
- Recovery trajectory and natural history over longer periods of time.
- Presence and prevalence of co-morbid conditions.
- Biomarker(s) to diagnose Long COVID.
- Risk factors for Long COVID.
- Prevalence and outcomes of Long COVID by sex, gender, race, ethnicity, socioeconomic status, and other factors.
- Patterns in Long COVID among special populations such as older adults; children and adolescents; pregnant, lactating, and postpartum persons; people with disabilities; people experiencing homelessness; tribal communities; and imprisoned populations; among others.
- Longitudinal consequences (e.g., risk and development of other diseases, disability, hospitalization, and death).
- Effects on functionality and daily living, overall well-being, and caregivers and families.
- Social sciences research aimed at understanding the social and economic consequences of Long COVID.
- New treatment and management options that could potentially affect the sensitivity threshold and elements of the definition.
CONCLUDING REMARKS AND RECOMMENDATIONS
The committee confronted many difficulties in its efforts to define Long COVID—most prominently the challenge of balancing risks of false negative and false positive classification. By putting forth the 2024 NASEM Long COVID Definition, the committee hopes patients, clinicians, public health practitioners, researchers, and policy makers will be better equipped to cope with this continually unfolding health crisis. The committee also hopes to foster greater awareness, understanding, and support for those with Long COVID. To conclude, the committee recommends three actions about the adoption, implementation, and updating of the 2024 NASEM Long COVID Definition (Box S-2).
BOX S-2
Recommendations
RECOMMENDATION 1. Adopt and Implement the 2024 NASEM Long COVID Definition.
The federal government, state, tribal, local, and territorial health authorities; clinical societies and associations; public health practitioners; clinicians; payers; researchers; drug industry; employers; educators; international organizations; and patients should adopt the 2024 NASEM Long COVID Definition and should use the term Long COVID. The 2024 NASEM Long COVID Definition is intended to be applied to many purposes, but the committee notes that there is flexibility within the broad definition, for example, to restrict research eligibility to a subset of Long COVID patients.
RECOMMENDATION 2. Promulgate and Monitor the Implementation of the 2024 NASEM Long COVID Definition.
The Office of the Assistant Secretary for Health’s Office of Long COVID Research and Practice and the Long COVID Coordination Council should lead the coordination and collaboration efforts across federal, state, tribal, local, and territorial agencies and other relevant entities, including international organizations, in the wide dissemination and implementation of the 2024 NASEM Long COVID Definition. Such implementation efforts should:
- Give special attention to the definition’s equity implications to maximize appropriate inclusion.
- Develop standardized communication for key stakeholders and the public about the revised definition and understanding of Long COVID.
- Empirically test the 2024 NASEM Long COVID Definition; monitor, evaluate, and identify barriers to implementation and adoption of the definition in research and in practice (including supporting
- an individual’s ability to apply for and receive Social Security disability benefits) that may be improved in future revisions.
- Develop a standard protocol for screening and diagnosing patients with Long COVID in clinical settings and enhance clinical education and training on infection-associated chronic conditions.
- Catalogue and summarize the application of the definition in research settings and identify sub-phenotypes of Long COVID that inform the need for further investigation across the translational research spectrum from discovery to delivery science.
- Take advantage of a unique opportunity to learn from epidemiologic surveillance of an infection-associated chronic condition and support, for example, improved data infrastructure, technologic and legal support for more efficient cross-jurisdictional information-sharing, and improved test types and access to testing.
RECOMMENDATION 3. Update the 2024 NASEM Long COVID Definition. In no more than 3 years or when triggered by the emergence of relevant new knowledge, the Office of the Assistant Secretary for Health’s Office of Long COVID Research and Practice should convene a multidisciplinary group, including individuals with lived experience, to reexamine and update the 2024 NASEM Long COVID Definition set forth in this report. The Office of the Assistant Secretary for Health’s Office of Long COVID Research and Practice should put into place the necessary infrastructure, policies, and mechanisms to support and prepare for future updates to the 2024 NASEM Long COVID Definition, including a process to track and assess new scientific knowledge that may inform the definition.
This page intentionally left blank.